American Indian adults have a diabetes prevalence of 15%, the highest of any racial or ethnic group. Their likelihood of dying from diabetes complications is more than 50% over that of their non-Hispanic White counterparts. Health-related quality of life is a measurement of health that encompasses physical, psychological, and social aspects of health and it has been to shown to be negatively impacted by type 2 Diabetes. A recent systemic review showed that the presence of complications, hypertension, depression, and type of diet were associated with worse health-related quality of life, however, American Indians were not included in this analysis. A new study explores the relationship between psychosocial factors and health-related quality of life for American Indians by describing functional social support, emotional support, coping, resilience, post-traumatic stress disorder, and health-related quality of life. It also investigates the association between psychosocial factors and health-related quality of life among American Indians living with diabetes.
Cherokee Nation is situated in Oklahoma and is one of the largest federally recognized tribes, with over 380,000 tribal citizens located on almost 7,000 square miles. From 2017 to 2019, the Cherokee Nation Public Health Department and the University of Oklahoma’s Sooner Survey Center conducted telephone surveys of users of the Cherokee Nation Health Services on health behaviors and issues. Data from this Cherokee Nation Health Survey was used in this study.
Public Health Impact
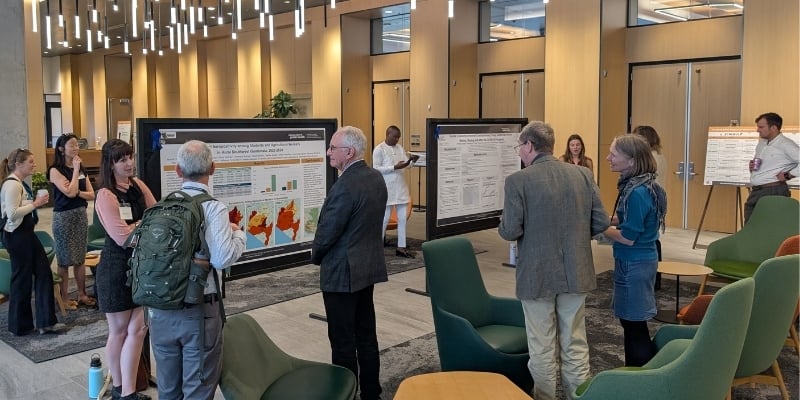
Spero Manson, Director of the Centers for American Indian and Alaska Native Health at the Colorado School of Public Health, and colleagues from around the country found that participants living with diabetes had lower social support and coping, and were more likely to report greater than 15 days of poor physical and mental health as compared to those without diabetes. Individuals who reported being dissatisfied or very dissatisfied with life were 6 times more likely to report poor overall health and those who had experiences of post-traumatic stress were twice as likely to report poor physical health. Higher resilience scores decreased the odds of reporting poor physical health.
This study demonstrates both risk and protective factors for diabetes outcomes in American Indian adults with type 2 Diabetes. It provides a foundation for future studies to examine the relationship between psychosocial factors and health-related quality of life in this population through pragmatic trials.