CDC officials on Tuesday warned that outbreaks of the novel coronavirus COVID-19 in the U.S. are likely, and that households, schools, healthcare providers and businesses should begin preparing. As part of this planning, it is important to recognize that protective resources and capabilities are not distributed evenly across the U.S. Public health protections are largely state and local responsibilities, provided through a constellation of public agencies and private organizations. In preparing for COVID-19, healthcare providers, first responders, and members of the public need to be aware of the emergency preparedness capabilities that exist in your area.
You can review detailed measures of emergency preparedness capabilities in your state and region using the National Health Security Preparedness Index. This index is the only national, longitudinal source of data on preparedness for the U.S. Because health security is a responsibility shared by many different stakeholders in government and society, the Index combines measures from more than 60 sources and multiple perspectives to offer a broad view of protection. Aggregating large volumes of data from national household surveys, medical records, safety inspection results, and surveys of health agencies and facilities, the Index produces composite measures of health security for each U.S. state and the nation as a whole. The Index reveals strengths as well as vulnerabilities in the protections needed to keep people safe and healthy in the face of emergencies, and it tracks how these protections vary across the United States and change over time. An overview report on the latest Index data and results is available online.
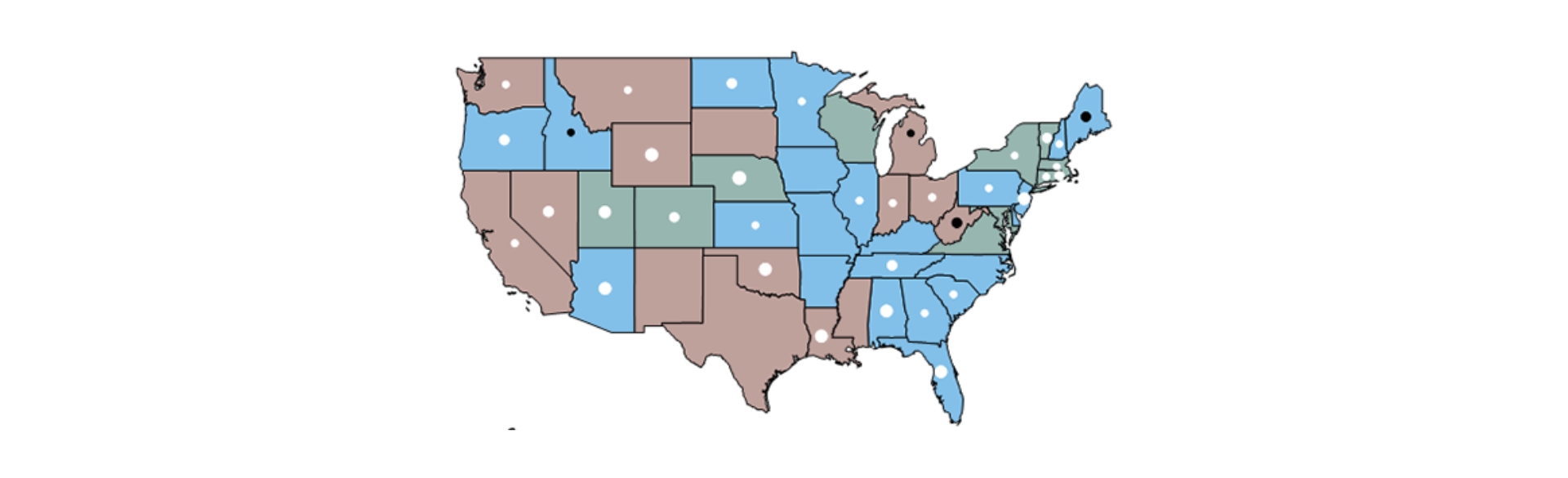
Data from the Index indicate that readiness for disease outbreaks and other emergencies has been improving over time, but current levels of health security remain far from optimal. Large differences in health security persist across states and regions, with clusters of states in the South-Central, Upper Mountain West, Pacific Coast, and Midwest regions lagging significantly behind the rest of the nation. Growth in the frequency and intensity of health security threats may outpace growth in the nation’s health security protections in the years to come, resulting in greater risks to population health.
The Index includes measures of preparedness in 6 broad domains. Some of the ways to use these measures include:
- Surveillance: If you live in an area that scores relatively low in surveillance capabilities, testing and diagnostic capabilities for COVID-19 may be more limited. Public health and healthcare officials should prepare now for delays in screening and testing. Estimates of disease prevalence and spread may have greater uncertainty in these areas.
- Community planning and engagement: Areas that score lower in this domain have less robust communication and support relationships among healthcare providers, schools, employers and community based organizations. To strengthen these relationships, check to see if your organization is a member of the local healthcare preparedness coalition. Check to see if your organization has a preparedness plan, if it has been updated recently, if it has been reviewed and practiced among staff, and if it has been shared with neighboring and partnering organizations. Confirm if you are trained and registered as an emergency volunteer willing to be called up if needed.
- Incident management: Areas that score lower in this domain may require more time to implement emergency management protocols such as standing up local emergency operations centers and establishing emergency communications and data sharing protocols across healthcare providers. Consider initiating these protocols as early as possible to allow for more time in working out bottlenecks.
- Healthcare delivery: Areas that score lower in this domain may face more challenges accommodating surges in demand for care at emergency rooms, hospitals, physician offices and pharmacies. Because COVID-19 disproportionately affects older adults, check to see if nursing homes in your area are connected to their local healthcare preparedness coalitions as sources of information, planning and support.
- Countermeasure management: Areas that score lower in this domain may face greater difficulties in accessing and distributing protective supplies and equipment such as masks, gloves, antivirals, and vaccines. Responders in these areas should plan now for how to access supply stockpiles and identify alternative sources.
- Environmental and occupational health: Areas that score lower in this domain may have fewer resources available for keeping workers safe and on the job during an emergency. Employers and employees in these areas should check their ability to work remotely and access paid time off benefits in the event of a widespread outbreak.
The National Health Security Preparedness Index was created with support from the U.S. Centers for Disease Control and Prevention in collaboration with national public health organizations, and is produced with funding from the Robert Wood Johnson Foundation. A research team at the Colorado School of Public Health, University of Colorado Anschutz Medical Campus, is responsible for producing and analyzing data for the Index, led by professor Glen Mays. More information and data are available at www.nhspi.org.
This story was originally written for Public Health Economics.



-Jul-14-2024-05-26-15-0673-PM.jpg)
-4.jpg)