A University of Colorado School of Dental Medicine faculty member is using his background in engineering to help alleviate the country’s shortage of ventilators in light of the COVID-19 crisis.
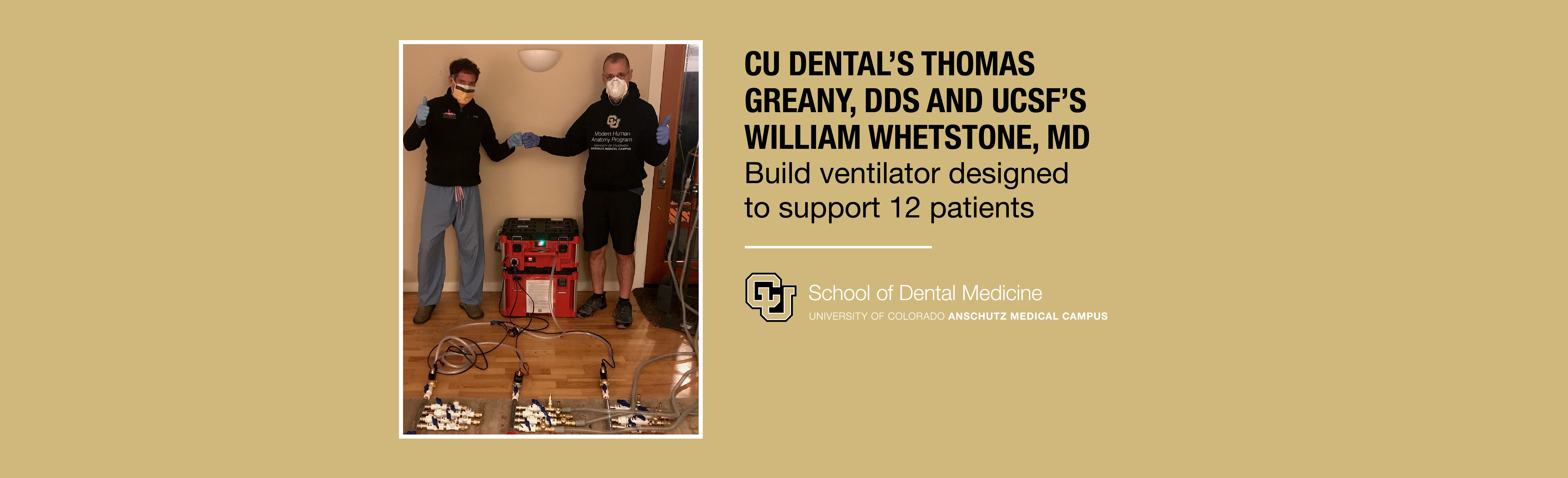
Thomas Greany, DDS, who received his undergraduate degree in aerospace engineering, was approached by a former CU Boulder roommate and engineering classmate William Whetstone, MD, a University of California San Francisco professor of emergency medicine, about whether he could build a field ventilator that would provide essential respiratory support for multiple patients simultaneously. Greany’s unit is designed to support 12 patients at a time with different inhale-exhale rhythms.
In many cases, the novel coronavirus attacks a person’s lungs, causing patients to feel as though they’re drowning. As an emergency physician, Whetstone knew that his hospital in San Francisco—and other healthcare facilities around the country might not have enough ventilators to treat a considerable influx of patients. Neither he nor any of his ER colleagues wanted to be in a position of having to refuse ventilation for any patient based on social value or randomization.
Within two weeks, Greany had designed and built a prototype model using a high flow commercial aquarium pump, which allowed for a continuous flow of air. He realized that other types of emergency ventilators known as bag-style vents have between one- and three-seconds delay for patients to exhale, but if a continuous flow system was used then, additional patients could be hooked up to the device.
“In my entire career, there’s been nothing more gratifying than the work that I’ve been involved with over the past four weeks,” Greany says. “It took a couple dozen energetic, enthusiastic and very special people to make it happen.”
Greany has been collaborating with another CU engineering alumnus, Ken Lambrecht, who created the project website, FieldVent.org. Steve VanNurden, MBA, CU Anschutz Associate Vice Chancellor and CEO of the Fitzsimmons Redevelopment Authority, connected the group to engineering design firm RK Mission Critical to build six of these emergency backup ventilators, which Greany dubbed, “Mother Mary, the Mother of All RespiratorY Devices.”
RK Mission Critical Tour
Patients connected to a traditional hospital ventilator in a chain must have the same breathing pattern—inhaling and exhaling roughly the same volume of air. Greany says he designed MARY to allow different types of patients—both conscious and fully intubated to be connected to the same pump and inhale different volumes of air thanks to a unique design.
As a faculty member, Greany uses his engineering background in CU Dental’s haptics lab—performing load simulations on teeth. The research allows dentists to predict how a particular type of drilling will affect the integrity of a tooth; and whether a damaged tooth will be strong enough to restore.
“My department chair, Dr. Dan Wilson, and Dean (Denise) Kassebaum have always been very supportive of the work I’ve been involved with, including the MARY device,” he says.
UC Health and CU Medicine each will receive a Mother MARY to test and deploy in emergencies. The Food and Drug Administration (FDA), which regulates ventilators, recently issued guidelines to allow for such backup devices to meet the ventilator shortage in the U.S.
“My ER physician colleagues have indicated that this device could have a significant impact globally, especially in developing countries that don’t have ventilators,” Greany says. “If nothing else, this pandemic has exposed a critical strategic shortfall in personal protective equipment and invasive ventilators worldwide.”
Once the COVID-19 pandemic runs its course, Greany believes the final step would be to obtain FDA approval for the device and introduce it to the developing world. The research team has already received support from CU Anschutz research leadership. Greany expressed tremendous gratitude for those who contributed to the project and especially those who bravely battle the pandemic on the front lines.