In the course of her research, Jamie Burke, a student in the University of Colorado School of Medicine, learned that at least 50% of patients surveyed at a safety net breast surgical oncology clinic were uncomfortable interpreting their own medical results.
This is a serious concern for many reasons, and may be the result of myriad factors, but at this early stage on her medical career she is recognizing the responsibility she and her colleagues share in becoming community partners to address this issue.
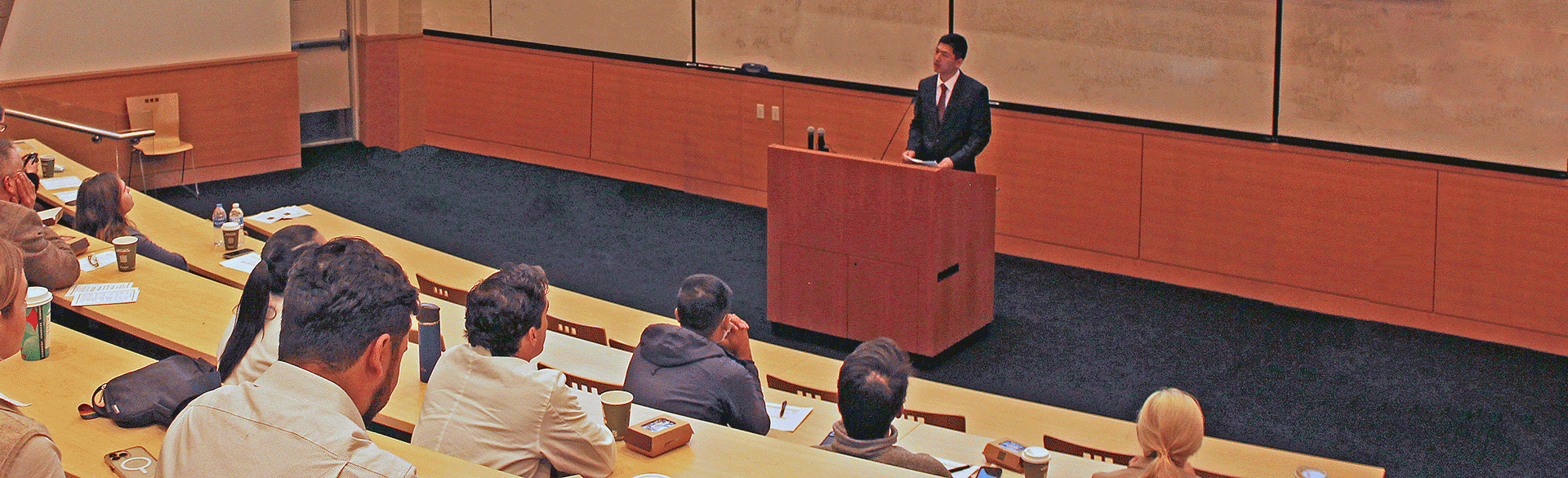
Burke was one of 13 participants in the CU Department of Surgery Medical Student Summer Research Program, who for two months over the summer worked with Department of Surgery mentors to conduct original research. They presented their research findings in five oral presentations and eight poster presentations at a symposium Dec. 12.
Program participants’ research delved into topics as varied as health literacy among patients in safety net clinics to cannabis use and postoperative outcomes in patients undergoing hepatectomy, opioid prescribing trends, and mortality rates among patients with COVID-19 infection and stroke, among others.

Medical student Catherine Alder presents research on preoperative variables and postoperative complications associated with outpatient mortality.
The program originated with Sarah Tevis, MD, an assistant professor of surgical oncology in the CU School of Medicine, who was inspired by her experience mentoring an undergraduate student through an eight-week summer research project. Expanding the curriculum she developed for her mentee to include lectures and clinical observation, Tevis partnered with Nicole Christian, MD, an assistant professor of surgical oncology in the CU School of Medicine, to lead the program.
Big approaches to find solutions
For Burke, who worked with mentor Tevis, that research included distributing surveys to adult female patients at a breast surgery clinic in a safety net hospital. The questionnaire, which was available in English and Spanish, asked not only demographic information, education level, and health insurance type, but questions about health literacy and perceived barriers to care.
Among respondents, 24% cited an inability to find transportation and 13% an inability to take time off work as significant barriers to accessing care.
After presenting her research findings to symposium attendees, Richard Schulick, MD, MBA, chair of the CU Department of Surgery, asked Burke, “How do we fix this?”
“Whether it’s offering ride sharing or having medical interpreters, these are not perfect solutions,” Burke said. “It will take a big approach because these tend to be populations who face a lot of closed doors and not a lot of people are opening them.”
Research leading to interventions
CU School of Medicine student Jason Sidrak, who conducted research with mentor Granville Lloyd, MD, an associate professor of urology in the CU School of Medicine, focused his research on improving attending health on the CU Anschutz Medical Campus via ergonomic interventions.
Sidrak’s preliminary analysis, conducted via an anonymous web-based survey sent to the CU Departments of Surgery, Anesthesia, Medicine, and Pediatrics, found that providers in the Departments of Surgery and Pediatrics most frequently reported experiencing back and neck pain, and were most likely to suspect their careers of contributing to their neck and back pain.
While the main function of the research was to generate hypotheses to identify ergonomic disparities, Sidrak said, the ultimate goal for this quality improvement project is to catalyze ergonomic improvement across the medical campus.
“We’re hoping this will lead to developing targeted interventions, to extend career longevity, and ensure our providers are being able to serve the people of Colorado for years to come,” he said.
Emphasizing ongoing education
Monday’s poster presentations highlighted a variety of research topics, including research by medical student Maksym Goryachok, who worked with Tevis, evaluating opioid prescribing trends and refill requests in the absence of prescribing guidelines. After retrospectively analyzing patient data for five common operations, Goryachok found that a higher postoperative opioid prescription quantity may be associated with increased outpatient opioid use in the form of refills.
“Next steps are to look at the same data with the factors used to prescribe the opioids,” Goryachok explained, adding that creating prescribing guidelines for various surgical procedures potentially can reduce over-prescription. “But that can’t be the end-all, be-all. Each patient is unique, so we need to educate physicians and promote a multi-modal pain approach.”
Following the presentations, Tevis praised the 13 program participants for their dedication and hard work, and mentioned looking forward seeing them present their research at conferences. “I don’t know if you recognize the progress you’ve made in such a short of amount of time,” she said.
In top photo: Medical student Jun Ha Gu presents his research on factors impacting provider utilization of HER-based pathways


.png)
