Even before the COVID-19 pandemic, intensive care unit (ICU) beds were in limited supply, and the pandemic only exacerbated this growing concern. Since the pandemic began, ICU resources have been in such demand that clinicians across the United States and world have struggled to meet the need.
A particular concern for surgeons has been whether an ICU bed will be available for patients who may need one following surgery.
However, a team of clinicians and researchers from the University of Colorado Department of Surgery found a solution using a risk assessment system they developed eight years earlier. Their work shows that the likelihood for post-operative ICU need can be accurately determined for each patient before surgery. In turn, this allows clinicians to effectively plan hospital stays and avoid delays in patients’ care.
In recently published research analyzing surgical data from almost 35,000 patients, researchers found that when they input eight pre-operative variables into the Surgical Risk Preoperative Assessment System (SURPAS), the SURPAS model accurately predicted post-operative ICU use across nine surgical specialties.
“The idea for this project really came about when ICUs were getting overwhelmed with COVID,” says Robert Meguid, MD, MPH, an associate professor of cardiothoracic surgery in the CU School of Medicine. “We were looking to determine which patients needed surgery sooner and which operations we could safely do with the resources that were available.”
Creating accurate risk prediction
Meguid and his colleagues developed SURPAS so that surgeons and other clinicians could obtain accurate risk prediction models for several adverse outcomes following surgery. Prior to the development of SURPAS, pre-operative risk assessment was based largely on clinician experience.
With SURPAS, which Meguid and his colleagues developed as a free online tool available to everyone, clinicians enter eight pre-operative risk variables to predict 30-day adverse outcomes following surgery. The eight pre-operative risk variables include surgical procedure, patient age, functional health status (a measure of how independent a patient is in their activities of daily living), American Society of Anesthesiology physical status classification, whether the patient will be admitted to the hospital after surgery, practitioner specialty, and whether the procedure is an emergency.
After entering these eight variables, the SURPAS creates risk estimates based on national procedure data. It compares predicted individual patient risk to observed national average risk for the procedure the patient will be having for 13 30-day postoperative adverse outcomes such as unplanned hospital readmission, non-home hospital discharge, infectious complications, cardiac complications, and death.
Previous research demonstrated that the eight-variable SURPAS compared favorably with the 28-variable National Surgical Quality Improvement Program (NSQIP) risk assessment tool developed by the American College of Surgeons.
Assessing ICU need following surgery
"As the pandemic has progressed, and as we’ve been refining SURPAS over the last eight years, one of the things we realized would be helpful was anticipating the need for an ICU bed following surgery,” Meguid says.
Paul Rozeboom, MD, a general surgery resident who conducted the research with Meguid and his research team, says that a goal of the data analysis was to determine whether a patient is low, intermediate, or high risk for needing ICU resources after surgery. “That’s a really important piece for having an informed discussion with patients before surgery,” Rozeboom says.
Analyzing data from about 35,000 patients in the UCHealth system between 2012 and 2018, Rozeboom, Meguid, and their co-researchers entered the patient data into SURPAS to see how accurately the eight SURPAS variables predicted ICU use.
Researchers found that the SURPAS model accurately predicted ICU bed use compared with observed local data.
By adding ICU need as one of the 30-day adverse outcomes in SURPAS, “it allows us to be better at planning, and it allows me to better communicate with patients,” Meguid explains. SURPAS also creates easy-to-understand data visualizations that compare a patient’s individual risk for adverse outcomes with the national average risk for those outcomes following the procedure they’re going to have.
A shared decision-making tool
“We’re pleased to see that the model we’ve been using for all these other complications, a model that can take fewer than two minutes to fill out for the average provider, is really accurate,” Meguid says. “Adding ICU need to a patient’s risk assessment is a really important piece in having a conversation with a patient and getting true informed consent.”
Because SURPAS allows clinicians to give patients a printed handout with their visualized risk assessment, “sometimes a patient will say, ‘I’m so much lower risk than I thought I was,’ or some may say, ‘I’m higher risk than the national average, and that makes me think about other options, maybe getting my affairs in order.’ We’ve learned from focus groups and surveys that patients are relieved knowing their risks, and that they want to be partners in care. They want to be engaged, and being more informed about risk can help decrease anxiety before surgery.”
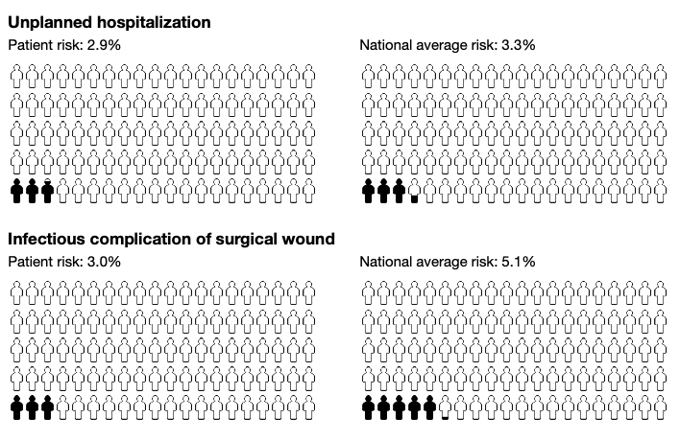
An example of visualized data from a patient risk assessment handout, comparing individual patient risk with national average risk
Rozeboom emphasizes that the SURPAS risk assessment is not meant to replace a clinician’s experience or expertise. “It’s a decision-making tool,” Rozeboom says, “a patient-facing shared decision-making tool. It’s something that’s visible to a patient to help them make a decision.”





.png)
