Since receiving FDA approval in 2017, chimeric antigen receptor (CAR) T-cell therapy has shown remarkable success in treating patients with certain blood cancers such as lymphoma and leukemia. A complex biomanufacturing process is required to produce the therapy, which is performed for each individual patient. The process begins with apheresis, generating a leukopak containing the patient’s white blood cells. From there, T cells are isolated, genetically engineered to create CAR proteins that enable T cells to attack cancer cells, and multiplied in a laboratory. They are then reintroduced to the patient.
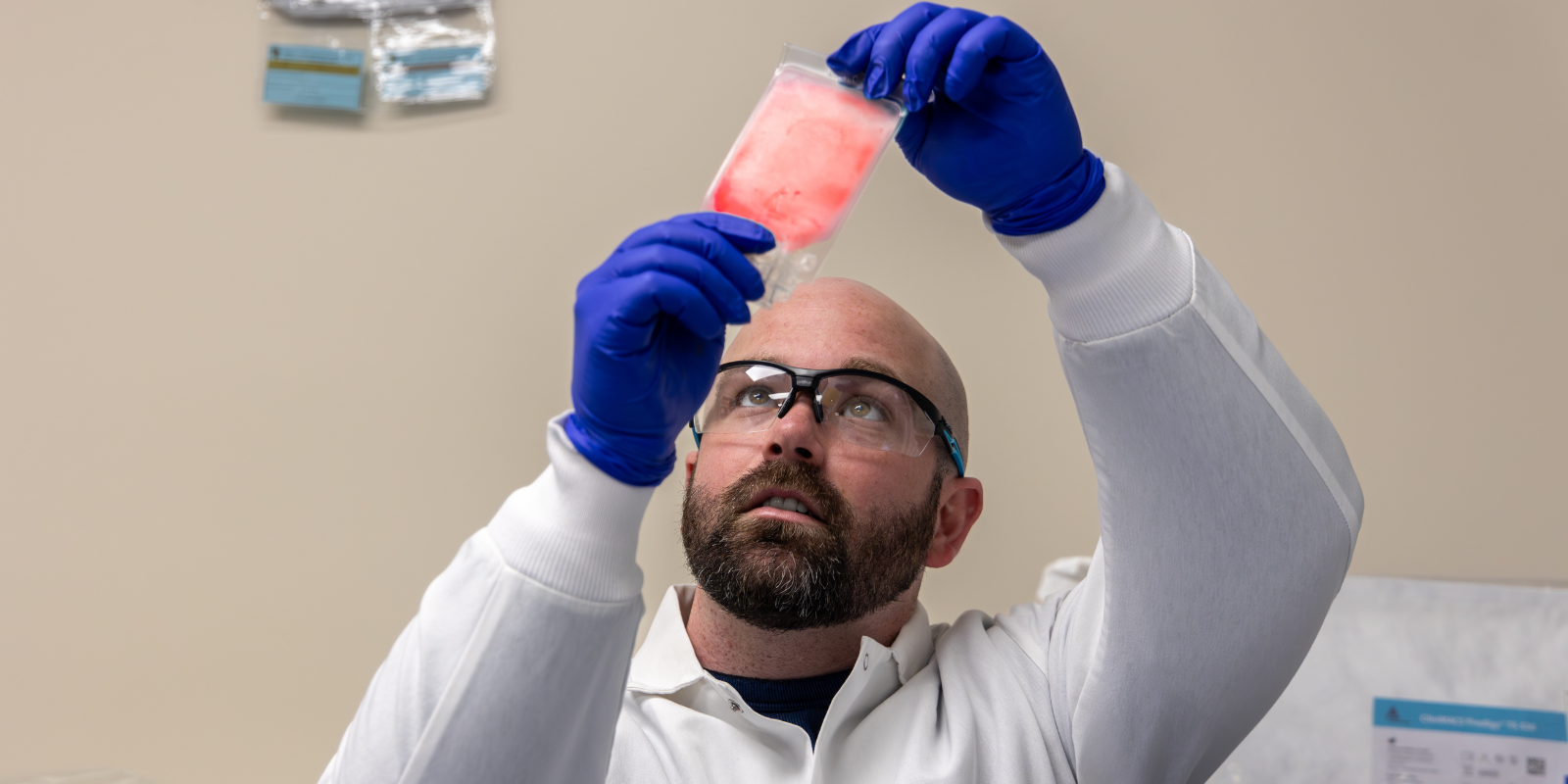
Until recently, manufacturing at Gates Biomanufacturing Facility (GBF), a pillar of the Gates Institute, began with a patient’s freshly drawn leukopak, typically received within 24 hours of apheresis, as a source of cells for the manufacturing process. However, the GBF has been testing techniques using cryopreserved leukopaks as a starting point, which could have far-reaching implications – for researchers, clinicians, and patients. Because CAR T-cell therapy is typically implemented after a patient has relapsed following chemotherapy, being able to cryopreserve healthy white blood cells before chemotherapy could improve outcomes. In addition, using cryopreserved cells could ease some of the logistical challenges of scheduling, shipping, and biomanufacturing processes, says GBF Executive Director Matt Seefeldt, PhD.
"Starting from cryopreserved starting material allows the clinic to ‘archive’ the blood prior to any chemotherapy for the patient, so the cells will be in a healthier state,” says Seefeldt. “In addition, the fresh blood expires 48 hours after the patient apheresis, so starting from cryopreserved cells allows the GBF and the clinic to have flexibility in its scheduling."
In 2022, Seefeldt and cell process engineer Benjamin Skinner began testing cryopreserved leukopaks donated by healthy individuals.
“The thaw process was designed to overcome two different mechanisms of poor cell recovery: coagulation and thaw-induced cell death,” says Skinner. “Coagulation would cause cells to be trapped as part of the normal clotting cascade, which initiates as the product thaws. Immediately after thaw, the cells are fragile and sensitive to osmotic stress. Moving cells from the solution they're frozen into, and then transferred into the solution needed for manufacturing is enough to kill a large portion of the cells unless that process is performed carefully.”
Regulatory approval was required before using CAR T cells made from frozen apheresis in an actual patient, says Cheri Adams, MSHS, program director of Regulatory Strategy at Gates Institute. “This meant amending the investigational new drug application to include the use of cryopreserved cells,” she says. “To satisfy the Food and Drug Administration, the GBF had to show that the finished product had a comparable risk-to-benefit profile as a therapy produced with fresh apheresis.”
The first products were administered in September 2023 to pediatric patients with B-cell lymphoblastic leukemia enrolled in a phase 1/2 trial of a CD-19 CAR T cell (UCD19) at Children’s Hospital Colorado.
“A lot of work has been put into it making sure the cells are viable,” says Seefeldt. “This is a significant manufacturing improvement, which will enhance cell and gene therapy research at University of Colorado Anschutz Medical Campus and benefit our pediatric patients who require manufacturing flexibility.”
.png)
-1.png)
.png)