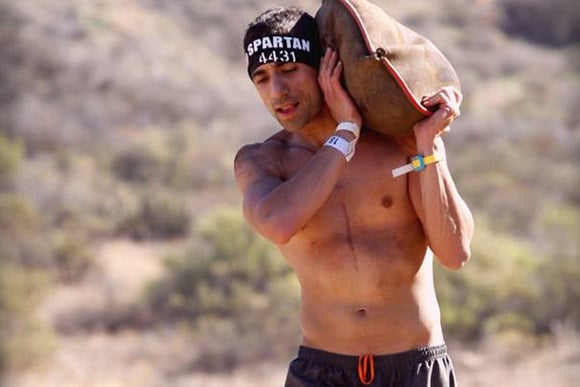
 Shabab Maslehati during the Spartan obstacle race
Shabab Maslehati during the Spartan obstacle race
From the time he was about 8 years old, Shahab Maslehati had been well aware that his chest was sunken. It had become more pronounced in adolescence, a time when, as he put it, "you're naturally self-conscious about everything." But it hadn't affected his high-school basketball career or his life in general into his early to mid-twenties. He graduated from Colorado State University in 2006 and took a job with the Farm Credit Administration in Denver, where he's worked ever since.
But by the time he and wife Kim had their son Imari in 2011, Maslehati sensed that something was wrong. He was short of breath, most noticeably when at rest. He felt lightheaded after walks up the stairs of his Aurora home. He figured he was just out of shape. He quit smoking. He started exercising. He got into very good shape, to the point that he competed in Spartan obstacle races, but just felt off when he wasn't exercising.
"I would be lying in bed and it felt like I was running," he said. "I was always trying to catch my breath."
He looked around online and came across a term he hadn't seen before, one that seemed straight out of ancient Rome: pectus excavatum. "Funnel chest," in the vernacular, is what he had.
 He doesn't have it anymore, thanks to the surgical handiwork of University of Colorado School of Medicine cardiothoracic surgeon Robert Meguid, MD, MPH, the support of his University of Colorado Hospital physical-therapist brother and others in his family, and a lot of hard work that has vaulted Maslehati into the best shape of his life.
He doesn't have it anymore, thanks to the surgical handiwork of University of Colorado School of Medicine cardiothoracic surgeon Robert Meguid, MD, MPH, the support of his University of Colorado Hospital physical-therapist brother and others in his family, and a lot of hard work that has vaulted Maslehati into the best shape of his life.
In late June, with a bar of surgical steel still implanted in his chest (it came out the following week), he finished the Salt Lake City Spartan Beast, a 13-mile obstacle race, in less than three hours.
PE
Pectus excavatum is the most common congenital chest wall abnormality, occurring in about one in 400 people. It's three times more common among males than females. While often noticeable at birth, severe cases typically happen with the growth spurt surrounding puberty. A related problem, pectus carinatum, (carinatum being Latin for "like a keel/hull"), in which cartilage overgrowth causes a protruding chest, is less than one-tenth as common. While the triggers of these chest-wall problems aren't known, extreme growth of the rib cage's costal cartilage is the cause.
 In many cases, there are no physical complications, Meguid said, although the chest's appearance can cause body-image issues and psychological stress. In addition to emotional impacts, severe cases can compress the space in the chest to the point that the heart can't completely relax and the lungs have less room to operate, resulting in shortness of breath and a diminished ability to exercise.
In many cases, there are no physical complications, Meguid said, although the chest's appearance can cause body-image issues and psychological stress. In addition to emotional impacts, severe cases can compress the space in the chest to the point that the heart can't completely relax and the lungs have less room to operate, resulting in shortness of breath and a diminished ability to exercise.
Pediatric surgeons at Children's Hospital Colorado perform as many as five corrective surgeries for these problems a month, Meguid said. But few surgeons in the region have expertise in the modified Ravitch procedure more commonly done to correct the condition among adults. Meguid, who joined the University of Colorado faculty in early 2012, now performs one or two Ravitch procedures a month at UCH.
Both the pediatric and adult procedures involve placing a steel bar under the rib cage, in effect tenting pectus excavatum or reeling in pectus carinatum. They differ in the specifics. The Nuss procedure, usually employed for children, is less invasive, using small incisions to insert and place the bar. The modified Ravitch procedure is open and, unlike the Nuss procedure, involves cutting and removing excess chest cartilage as well as splitting the sternum horizontally. Adults having undergone the Ravitch procedure see the steel bar removed in about six months, Meguid said; pediatric patients retain the Nuss procedure bar for two to three years.
Severe case
Yet despite these treatments, pectus excavatum remains poorly recognized in the medical community. Maslehati bounced around for about two years – his primary care physician dismissed the notion of his chest being a problem until a California practice he came across on the Web suggested a couple of specific tests that showed his case to be severe – before he finally landed a referral with Meguid in mid-2013.
Maslehati was a good candidate for surgery, Meguid told him, though the doctor suggested waiting until after Maslahati's wife delivered their second child. Maslehati wouldn't be allowed to lift more than 10 pounds for eight weeks after surgery.
Ivy was born in October 2013; Meguid operated on Maslehati in mid-December. Maslehati woke up in pain – the epidural had numbed one side better than the other. But that wasn't the dominant sensation.
"I took a deep breath like I never could before," he said. "My first thought was: 'This is what it's like to breathe.'"
He recovered at UCH for five days. When he went home, he had to sleep in a sitting position. A cough or sneeze brought on excruciating pain. He wouldn't start official physical therapy until week 13, but Maslehati had an inside track: his younger brother, Arash Maslehati, PT, is a UCH outpatient physical therapist.
"I'd seen my brother go through his whole life with this, and I saw how it affected him," Arash said.
The first thing Arash taught his brother was how to roll over so he could get out of bed, Shahab said.
New peak
 It was a tough rehabilitation. The chest is rife with rib joints and muscles, many of which in essence "turn off" following surgery and need prompting to reengage, Arash said. Shahab's chest muscles had been disconnected during the procedure, so he couldn't do a single push-up. In the first six weeks of formal rehab at UCH, Arash worked with individual muscle groups and later combined them. Postoperative principles of healing and biomechanics guided the processes, he added.
It was a tough rehabilitation. The chest is rife with rib joints and muscles, many of which in essence "turn off" following surgery and need prompting to reengage, Arash said. Shahab's chest muscles had been disconnected during the procedure, so he couldn't do a single push-up. In the first six weeks of formal rehab at UCH, Arash worked with individual muscle groups and later combined them. Postoperative principles of healing and biomechanics guided the processes, he added.
"We want things to mend, scar down, and also augment that healing," Arash said. His brother's case got him interested in chest wall disorders to the point that Arash has become the hospital's go-to chest wall PT, he added.
Shahab's exceptional fitness before surgery contributed to a speedy recovery. Arash said his brother was back to near-normal in three months, roughly twice as quickly as a typical case.
"You've got to go into that surgery being at your absolute peak, or as close to your peak as you can, and then you're going to recover way faster," Shahab said.
He had an inside track on an excellent physical therapist, but even those lacking such family connections should seek one out before surgery, he said. After the surgery, focus on the small milestones, he said, rather than thinking about where you were beforehand.
"Dr. Meguid is a huge, absolutely critical part of where I am today," he said. "But if you're not on board, people can't just fix you."
Meet the New Clinic
The CU Department of Surgery's new Multidisciplinary Chest Wall Disease Management Clinic focuses on a range of chest wall problems spanning adult and pediatric patients. Cardiothoracic surgeon Robert Meguid, MD, MPH, who specializes in chest wall surgeries, saw the need to create a clearinghouse of chest-wall expertise spread about the Anschutz Medical Campus. He and pediatric surgeon David Partrick, MD, serve as co-directors.
"The aim of the multidisciplinary team is to have a one-stop shop for patients," Meguid said. "In the past, they've bounced around, and there's been a lot of difficulty and frustration in getting to the right provider."
The clinic, for now an informal group, includes experts in congenital problems such as pectus excavatum, pectus carinatum, pectus acuatum, Poland syndrome, and cleft sternum; acquired chest wall disease, such as chest wall tumors and chest wall infections; chest wall trauma; and thoracic outlet syndrome. As patient demand continues to rise, Meguid said he would like to establish a formal monthly meeting of the minds in the same vein as the pancreas, lung cancer, GI, and other multidisciplinary clinics at UCH.
The Multidisciplinary Chest Wall Disease Management Clinic Team:
Thoracic Surgery
- Robert Meguid, MD, MPH, FACS
- John Mitchell, MD, FACS
- Michael Weyant, MD, FACS
Vascular Surgery
- Charles Brantigan, MD,
- Natalia Glebova, MD, PhD
- David Kuwayama, MD, MPA
Pediatric Surgery
Plastic Surgery
- Frederic Deleyiannis, MD, MPhil, MPH, FACS
- David Mathes, MD, FACS
Congenital Cardiac Surgery
- David Campbell, MD, FACS
By Todd Neff
