Researchers at the University of Colorado Anschutz Medical Campus are part of an international team that has discovered a molecular signature that plays a pivotal role in sustaining the activation of immune cells in chronic neurological diseases, including progressive multiple sclerosis (MS).
The study was published today in the journal Nature.
Over 2 million people live with MS. And despite existing treatments, two-thirds of them transition into a debilitating secondary progressive phase of the disease within 25-30 years of diagnosis, leading to worsening disability.
In MS, the body’s own immune system attacks and damages myelin, the protective sheath around nerve fibers, disrupting messages in the brain and spinal cord. In progressive forms of the disease, macrophages, white blood cells that digest pathogens, and microglia, brain and spinal cord cells that fight invaders, attack the central nervous system (CNS), causing chronic inflammation and damage to nerve cells.
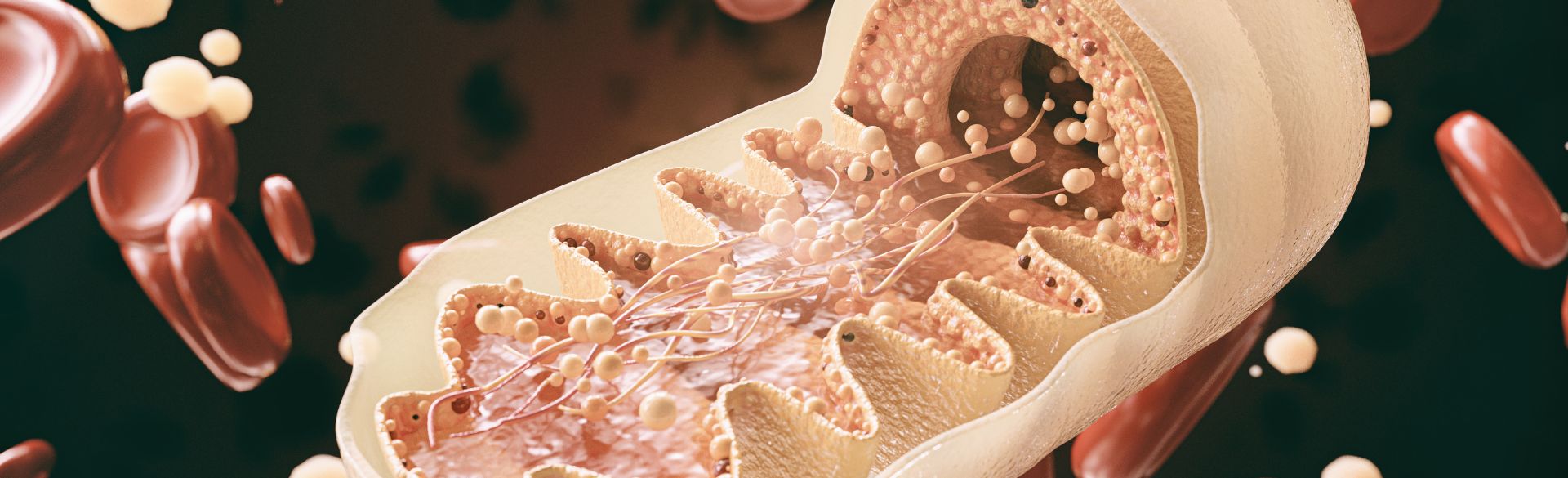
Scientists from Cambridge in collaboration with the CU School of Medicine, have found that how microglia use their mitochondria, the primary energy generator of the cell, determines their persistent state of activation, leading to irreversible neuronal damage and neurodegeneration.
The findings provide crucial insights into the metabolic underpinnings that perpetuate inflammation in chronic neurological diseases.
Scientists unravel mitochondria effect
"Our work unravels a previously unrecognized aspect of microglial activation in progressive MS,” said Professor Stefano Pluchino, MD, PhD, from the University of Cambridge, who co-led the study. “By targeting mitochondria, we may have identified a promising therapeutic strategy to mitigate damage to nerve cells and improve functional outcomes in progressive MS and potentially other neurodegenerative diseases.”
The research team discovered a novel molecular pathway involving mitochondrial complex I (CI) activity, reverse electron transport (RET), and the production of reactive oxygen species (ROS), providing crucial insights into the metabolic underpinnings that perpetuate inflammation in chronic neurological diseases.
The scientists also demonstrated the therapeutic potential of their findings by blocking CI in pro-inflammatory microglia, leading to neuroprotection in animal disease models.
The breakthrough suggests that inhibiting CI activity in microglia could be a game-changing approach to treating chronic inflammatory CNS disorders, such as progressive MS. This opens the door to the development of targeted therapies that modulate microglial activation and promote neuroprotection.
As part of this study, the lab of Angelo D’Alessandro, PhD, a professor at the CU School of Medicine, performed mass spectrometry-based analyses of immune cells from the mouse brains in a model of experimental autoimmune encephalomyelitis.
Lab paves way for future studies
"Having developed extremely sensitive methods that allow us to characterize metabolism in extremely low cell count populations, we were uniquely positioned to contribute to this collaborative project,” D’Alessandro said. "Our data show that immune cells from this model are characterized by elevated markers of oxidant stress and dysfunctional mitochondrial metabolism in vivo, paving the way for studies on the efficacy of interventions aimed at blocking a novel mechanism of mitochondrial dysfunction, called Reverse Electron Transport (RET).”
Cambridge's Luca Peruzzotti-Jametti, MD, PhD, first author and co-lead of the study, anticipates the relevance of this discovery and the still unmet need of translating these research findings into tangible benefits for individuals living with chronic neurological diseases.
“Our discovery represents a significant step forward in our understanding of the complex interplay between mitochondrial metabolism and inflammation in the brain. As the research community eagerly awaits new treatments, the potential for a new class of therapies targeting mitochondrial CI activity in microglia offers hope for improved outcomes and a brighter future for those affected by chronic neurological disorders,” Perizzotti-Jametti said.
This work has received funding from the Bascule Charitable Trust, European Committee for Treatment and Research in Multiple Sclerosis (ECTRIMS), the Evelyn Trust, Fondazione Italiana Sclerosi Multipla (FISM), the Isaac Newton Trust, the National MS Society, the UKRI Medical Research Council, the U.S. National Heart, Lung and Blood Institute, the U.S. National Institute of General and Medical Sciences, the UK Dementia Research Institute (UKDRI), the Wellcome Trust and Wings for Life.