With the August approval by the Food and Drug Administration of a new therapy to treat young patients with a form of leukemia, the University of Colorado Anschutz Medical Campus is positioned to contribute to a revolution in patient care.
The therapy, from Novartis, carries an exotic name that is bound to become more familiar in the days ahead: chimeric antigen receptor T cell, or CAR-T. It’s not a drug or radiation, but rather a new line of attack that relies on reengineering a patient’s own cells to recognize, attack and kill cancer cells. The target in the Novartis therapy is acute lymphoblastic leukemia (ALL), the most common form of cancer in children.
The trial of the therapy, called Kymriah, targeted ALL patients 25 years or younger with high-risk leukemia who relapsed after standard therapy, including bone marrow transplants and chemotherapy, or whose disease was resistant to treatment. More than 80 percent achieved remission within one month of therapy. The longest TCAR treated patient is more than five years from treatment and she remains in remission.
“It’s a tremendous leap forward,” said Lia Gore, MD, head of Pediatric Hematology, Oncology and BMT at Children’s Hospital Colorado. “It’s a landmark change in how we will treat disease, in this case cancer.”
Children’s Colorado is one of 30 or so hospitals nationwide approved to administer the Kymriah therapy. Treatment will not be available outside an approved center.
Seek and destroy
Gore is principal investigator in a separate trial of a similar immunotherapy from Kite Pharmaceutical. Like Kymriah, the Kite therapy takes a page from nature’s book to turn the tables on cancer. Both treatments target a protein called CD19 that ALL cells commonly express. Clinicians harvest T-cells, key building blocks of the body’s immune system, from the patient then send them to a facility where they are genetically modified, grown, and expanded in the lab under special conditions. In effect, the T-cells are retrained to seek, identify and destroy an enemy – in this case the cancer cells marked by CD19.
The manufacturing facility grows the reengineered cells by the millions, then ships them back to hospital clinicians, who infuse them back into the patient in a process similar to a blood transfusion. The cells grow and expand in the patient, and the immune system uses its newly weaponized T-cells to not only fight the cancer but in an encouraging number of cases rid itself of it.
“It works somewhat like a vaccine, in that the body mounts an immune response to the cancer cells," Gore said.
Promising as it may be, don’t look for immunotherapy clinics to sprout in strip malls. Nor is the treatment, or the body’s response to it, akin to routine vaccination.
“It requires a high level of expertise,” Gore said, including teams to collect the blood cells, equipment to store and ship them, a dedicated lab to generate the cells and return them to clinicians to infuse the reengineered cells, and expertise to manage patients who receive the therapy – which is not without risks of its own.
One serious side effect of the therapy, for example, is cytokine release syndrome, a reaction to the specialized T-cells that can drive dangerously high fevers, low blood pressure, fluid retention, and neurologic problems, Gore said. The reaction is “evidence that the immune system has been activated to try to fight the cancer cells,” she added – a good thing – but it will frequently require intensive care.
Patients who receive the therapy also require extensive follow-up care, noted Kelly Maloney, MD, program leader for Leukemia/Lymphoma at Children’s Colorado. Maloney manages follow-up care for several patients who participated in the Novartis trial at other hospitals. The follow-up includes monitoring blood counts as well as liver and kidney function, and providing follow-up reports to the trial-site hospitals. Patients also require lifetime immunoglobulin infusion therapy to replace healthy infection-fighting cells that are killed along with cancer cells by the CAR T-cells, Maloney explained.
New hope
While the complexities make for a clinical challenge, the selection of Children’s Colorado as an approved site for the Kymriah therapy is an exciting prospect for young patients and their families, Maloney said. Kymriah has produced remarkable remission numbers in kids who have frequently relapsed, leaving them with slim hopes of recovery, she said.
“For years and years, we’ve seen kids relapse after their first remissions,” said Maloney, who finished her fellowship training in 1998. These tough cases have required bone marrow transplants and multiple, increased doses of chemotherapy in attempts to turn the tide.
“In the past, with these multiply relapsed patients, there was nothing left for us to offer,” Maloney said. “It’s easier to have glimmers of hope now for families. The therapy is likely to move earlier in therapy in some patients so it’s not going to come with second and third and fourth relapses. It’s going to move up to a targeted, first-relapse therapy.”
 Cells in a biosafety hood in the Verneris Lab. The flasks contain T cells and natural killer cells that have been growing in the laboratory under various conditions for two or three weeks.
Cells in a biosafety hood in the Verneris Lab. The flasks contain T cells and natural killer cells that have been growing in the laboratory under various conditions for two or three weeks.
“The future is very bright for these patients,” agreed Michael Verneris, MD, program leader of BMT and Cellular Therapy at Children’s Colorado. Verneris was the local principal investigator for the Novartis trial at the University of Minnesota before moving to Colorado late last year.
The 80-plus-percent remission rates for the trial patients are especially notable because their conditions were so grave, Verneris said. “Kids enrolled in this trial had life spans that we measured in weeks and months,” he said.
Home-grown, natural-born killers
The CU Anschutz Medical Campus is poised to become a bigger player in the burgeoning immunotherapy field, Verneris said. For example, it’s home not only to the researchers and clinicians who will drive new therapies forward but also to the biotechnology facilities capable of growing the massive stocks of blood cells necessary to administer the therapies.
Those players include Children’s Colorado – and, on the adult side, UCHealth University of Colorado Hospital – the CU School of Medicine; Clinimmune Labs, a massive blood collection, processing and storage facility owned by CU; and the Gates Center for Regenerative Medicine, which is supported by CU Anschutz, UCHealth and Children’s Colorado. The center conducts the stem cell research and biomanufacturing that helps to drive the development of immunotherapies and other cell-based approaches to treating disease.
The search for the next-generation of cancer therapies is also underway in Verneris’s lab on the fourth floor of Research Complex 1 North at CU Anschutz. He and his colleagues are working to transform simple skin cells into cancer-fighting warriors. The technology, developed about a decade ago, involves genetically reprogramming the cells to return them to their embryonic state. At this point, these induced pluripotent stem cells (iPSCs), as they’re called, are blank slates awaiting an identity through genetic prodding.
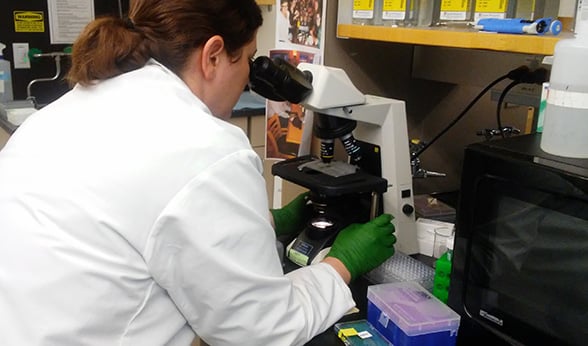 Jessica Lake, MD, a pediatric hematology/oncology/bone marrow transplant fellow at CU, counts natural killer cells before an experiment in the Verneris Lab.
Jessica Lake, MD, a pediatric hematology/oncology/bone marrow transplant fellow at CU, counts natural killer cells before an experiment in the Verneris Lab.
Verneris is working to create white blood cells called natural killers (NKs) from iPSCs. In the body, NK cells detect and destroy cells in the body that have been altered and thus pose a threat. Their targets include cancer cells. In the lab, Verneris and his team are growing their own NKs from iPSCs and testing their cancer-killing power. The goal: create a potent weapon that can be mass-manufactured and infused in patients – an “off-the-shelf” therapy, as he describes it.
“Companies are charging toward this,” Verneris said. “It’s an incredibly exciting time.”
Wide application – and more questions
For Gore, the immunotherapy approach has great power because it can be broadly applied. Researchers are already looking at using it to fight acute myeloid leukemia, a form more aggressive than ALL, with a lower survival rate, she said. It’s being investigated to treat brain tumors, sarcomas and other cancers. Kymriah focused on CD19 because the protein is common in this type of leukemia, and therefore a good therapeutic target, Gore said, “but there are antigens on the surface of every cell.” Many of them could one day find themselves in the crosshairs of a patient’s newly charged immune system.
For now, however, a central question and challenge from the Novartis trial remains. Why did the Kymriah therapy work much better for some patients than others? It turns out, Verneris said, that in some, the CAR T-cells did not “persist.” That is, they worked well initially in killing the cancer cells, but then diminished in number, allowing cancer cells to reclaim the battlefield.
“The question is, where did they go in the body?” Verneris said. “We want them to stay in the blood.”
For that reason, Kymriah cannot be called a cure for everyone, Gore added. It’s a problem that requires ongoing research. One possible confounding factor, Gore said, is leukemia and other cancer cells’ ability to mutate and develop their own resistance mechanisms to fight off the CAR T-cells.
Because of these uncertainties and the quest for new knowledge about the disease and the people it strikes, clinicians and researchers will monitor Kymriah patients for at least 15 years, Gore said. “We need to evaluate its long-term effects.”
Paying the price
Another uncertainty and source of controversy is the cost of the therapy, pegged at $475,000 to hospitals directly. This charge does not represent the total cost to patients and insurers for receiving this therapy, Gore said, although Novartis has said the charge will be dropped if it doesn’t work in the first month.
Maloney acknowledged the issue of cost will be a point of contention but emphasized that it plays no role in her clinical decision making.
“My job as a physician is to provide the best therapy for my patients,” she said. “I can’t put the decision on a cost-benefit ratio. All my patients’ lives are precious and they all deserve the best chance of survival.”
A further complication is that some patients will require a bone marrow transplant after CAR-T therapy and some will not, Gore added. The cost of a transplant is roughly $150,000 to $200,000 at the low end, but complications and long-term care can drive that to $1 million and higher, she said. If, on the other hand, a patient doesn’t need a transplant after the CAR-T therapy, “the overall cost [of the therapy] is probably going to be less over a lifetime.”
For Verneris, that points to the need to identify as accurately as possible which CAR T-cell therapy patients will likely also need a transplant.
“We know that some patients have been in remission up to five years with CAR-T. They are probably cured,” he said. But for patients who had shorter remissions, the “door opens to BMT,” he added. “The challenge is figuring out who needs the transplant and who doesn’t.”
These questions don’t dampen the excitement that immunotherapy is generating in the pediatric hematology world at large or, especially, at Children’s Colorado, Maloney said.
“Having more access [to CAR T-cell therapy] and having a family able to stay local is super-important for the psycho-social part – having people around them who can support them for what can be a tough therapy at times,” she said.
