Immersive traumatic brain injury (TBI) treatment programs such as those provided by the Marcus Institute for Brain Health (MIBH) are helping millions of TBI patients through holistic and intensive care, but they are only “scratching the surface of the need” nationwide.
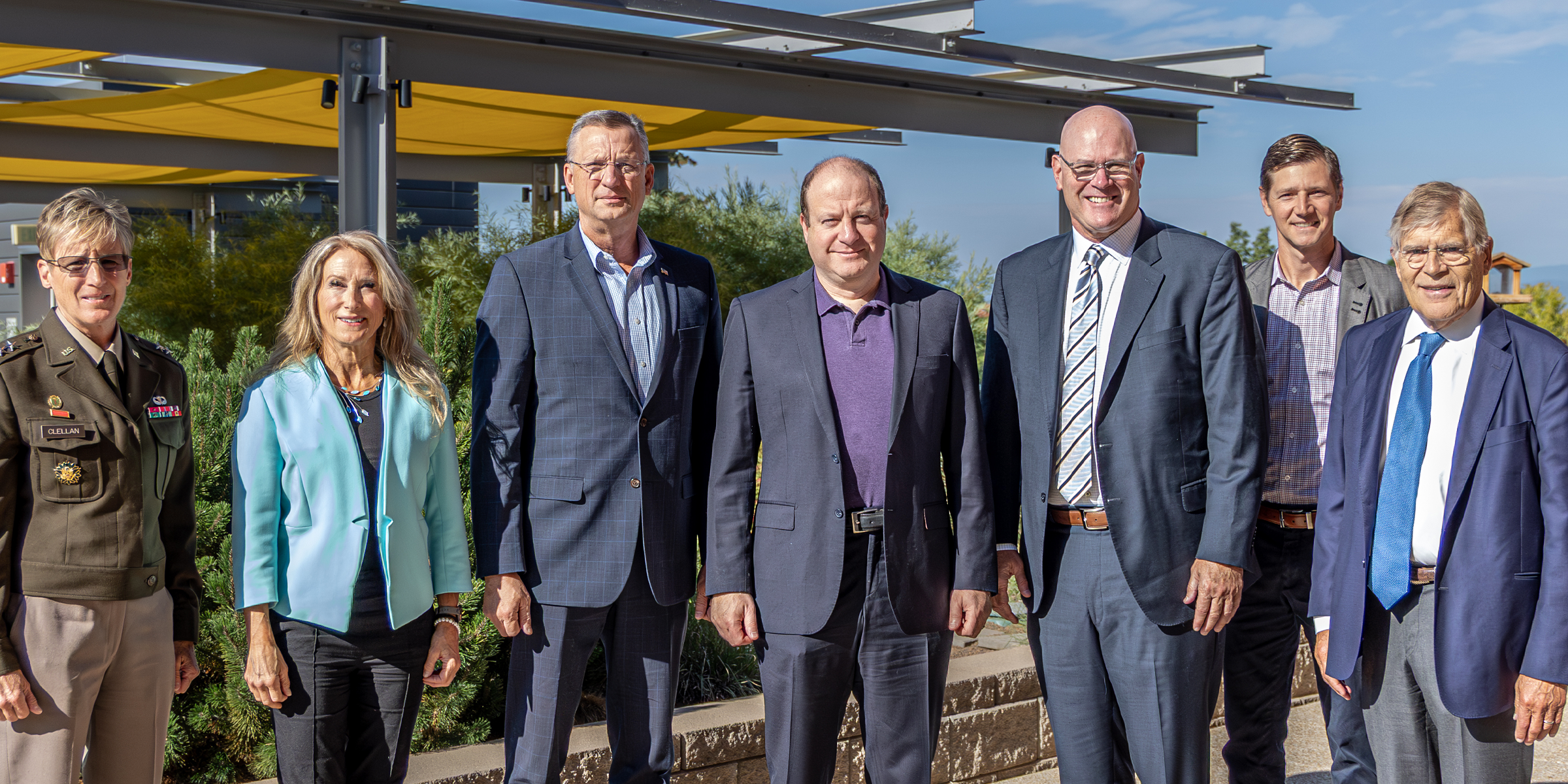
That was a key message conveyed to U.S. Department of Veterans Affairs Secretary Douglas Collins who visited the MIBH at the University of Colorado Anschutz Medical Campus on Monday. Collins and Colorado Gov. Jared Polis heard about the impact of the MIBH as well as an integrated national network of facilities that treat TBI, post-traumatic stress disorder and substance abuse.
Collins and Polis heard from Brig. Gen. Kathleen Flarity, DNP, PhD, executive director of the MIBH, and Joe Brennan, CEO of Avalon Action Alliance, a nonprofit that helps veterans, first responders and families address mental wellness and brain health issues. On a tour, they got a close-up look at the MIBH’s physical performance laboratory and creative arts therapy program.
‘Vital part of our mission’
CU Anschutz Chancellor Don Elliman told Collins that because of the campus’s historical ties to the military, leadership decided that “it would be an honor for us to be able to stand up something for TBI, and it’s proven to be just that. We’re fortunate to have Gen. Flarity running the operation now, but it is a vital part of the mission of this campus and the University of Colorado. We’re very proud of the results that our people have been able to achieve.”

Brennan explained that Avalon partners nationally with six traumatic brain injury facilities (including the MIBH), 11 post-traumatic stress centers and two substance abuse operations.
The collective centers’ intensive treatment programs are effective, he said, but also expensive. The average cost of a three-week TBI program is $42,000, down from $51,000 last year. Brennan and Marcus Ruzek, senior program officer at the Marcus Foundation, which contributed $38 million to launch the MIBH in 2017, noted that it’s imperative to make the treatment programs sustainable through improved insurance reimbursements, streamlined program scaling, increased private investment, and more state and federal government funding.
Building a workable business model
“Even if all six quality trauma centers were treating every veteran, and if the capacity of Avalon doubled or tripled today, we’d still be scratching the surface of need,” Ruzek said. “That’s the scope of this problem: We have over half a million people diagnosed with mild to moderate traumatic brain injuries in this population (veterans, active duty military, first responders, and Guard and Reserve personnel), so what needs to happen is creating a business model that works, so that eventually the free market can build capacity such that we can see everybody who needs it.”

Statistics show that 2.8 million Americans suffer from a TBI every year. According to Department of Defense statistics, suicides among active-duty personnel have increased since 2011, while the Guard and Reserve have remained mostly stable. Improving care for these patients is the core mission of the MIBH and COMBAT Center (University of Colorado Center for Combat Medicine and Battlefield (COMBAT) Research). Their role was highlighted by a recent CU Anschutz lecture titled “Military Medicine and the Mind: Bridging Battlefield Research and Civilian Care.”
Flarity said 79% of the patients served at MIBH are veterans. The facility does not require health insurance, and veterans and their families pay nothing out of pocket for the evaluation and outpatient programs.
“We know that the bigger our team, the more flexible and agile we are and the more throughput we can give,” Flarity said. “Since I’ve been in my position (she became executive director in February 2024), we’ve increased our throughput by 39% in the number of patients served.”
‘Top-of-the-game team’
In all facets – from initial evaluation to the intensive outpatient program to follow-up care, which in most cases is managed in partnership with a VA liaison – patients receive elite-level care, she said.
Polis asked how much training the treatment program clinicians receive to qualify as providers.
Many are trained neurologists, neuro-psychologists and other medical specialties. “We have 13 disciplines co-located and integrated,” Flarity said. “That’s the biggest cost: You have this expansive, top-of-the game team that are here to give all that care just to you, because every TBI is different. We’re giving that level of precision medicine here.”
When Polis asked about insurance reimbursements – either through TRICARE (the U.S. military’s healthcare coverage program) or private insurance – Brennan said they are modest. He said the goal is to get the three-week regimen cost down to $30,000, “which is pretty incredible, based on the care that someone gets.”
Patients at the MIBH can see up to 32 providers in various specialties in a single week, and many visits include being treated by two providers, with complementary skill sets, at the same time. “The current (reimbursement) model is not made for using 32 providers in a week,” Flarity said.
‘Life-altering’ care
She shared a couple patient testimonial stories that captured MIBH’s profound effect on patients’ lives. “Sir, for far too long traumatic brain injuries have been misunderstood and they’ve often been diagnosed as PTSD,” she told Collins. “If you never treat the underlying cause, the patient will never get better.”
Also misunderstood for decades is how TBIs extend well beyond service members who experienced a singular violent-blast event, she said. Low-level cumulative blast injuries sustained by mortarmen and other military specialties have been found to likewise cause TBIs. “So, we owe it to our nation’s heroes to figure out how to prevent and mitigate injuries – we have lots of ideas – but also owe it to them to treat them.”
MIBH’s integrated treatment program is built upon a whole-person concept, the director said.
“If you treat the whole person, all of those wellness practices that they can practice, it’s going to be life-long, it’s not going to be just here,” Flarity said. “And we don’t fix everything, but if we start them on that trajectory, then it’s life-altering.”
Colorado Congressional Leaders Introduce Traumatic Brain Injury Bill
Two of Colorado’s Congressional Representatives – Jason Crow and Jeff Crank – introduced legislation on July 10 that looks to bolster support for active-duty service members with traumatic brain injuries (TBIs). The legislation comes at an important time – hundreds of thousands of U.S. service members have been diagnosed with TBIs over the last two decades. The bill itself would set up a working group within the Department of Defense to examine how the latest digital health technologies could be used to help military service members struggling with TBIs.
Photo at top: Pictured from left are Maj. Gen. Laura Clellan, executive director of the Colorado Department of Military and Veteran Affairs; Brig. Gen. Kathleen Flarity, DNP, PhD, executive director of the Marcus Institute for Brain Health; VA Secretary Douglas Collins; Gov. Jared Polis; Joe Brennan, CEO of Avalon Action Alliance; Marcus Ruzek, senior program officer of the Marcus Foundation; and CU Anschutz Chancellor Don Elliman.