For Enrique Soto Pérez de Celis, MD, PhD, treating cancer globally starts with treating cancer locally.
“I was surprised to discover that the Latino population in Denver was over 30%,” says Soto, who moved to Colorado from his home country of Mexico in April to become the University of Colorado Cancer Center’s associate director for global oncology.
“I was even more surprised to know that we don’t have that many people from the Latino community coming to the CU Cancer Center,” he continues. “Part of the idea behind my new role is to continue building bridges with the local communities, and also to create a connection between local communities and the countries where they originally came from one, two, or three generations ago.”
Moving beyond charity
It’s all part of Soto’s approach to treating and researching cancer on a global scale, which looks a little different than it does at similar programs at other cancer centers in the U.S.
“In many cases, it’s looked at like a charity: ‘We go out and we provide care in places where people do not have care. We throw money at places where money is not available,’” he says. “But it should be seen as an opportunity for two-way collaborations. There are huge opportunities for researchers in the U.S. to conduct trials with partners from low- and middle-income countries to improve care there, but there also are opportunities to learn from the way things are done in low- and middle-income countries and bring it back here.”
For example, he says, in Mexico, patients may have to wait three months to get radiotherapy, so oncologists must come up with creative ideas to keep people from getting worse in the meantime. The process offers lessons for researchers and providers in the U.S. and elsewhere.
“It’s a concept I really love, which is reverse innovation,” he says. “We usually see innovation from top to bottom, like, ‘We are super-sophisticated; we’ll teach you how to do things.’ And that in many cases, fails. There are places in the world where people treat cancer for a fraction of the cost and the time it takes here. And there is a lot to learn from that. For researchers doing basic science, clinical science, and implementation science, having this global perspective is essential.”
From Mexico to California — and back again
Soto’s global perspective was honed during his residency and fellowship at the Instituto Nacional de Ciencias Médicas y Nutrición Salvador Zubirán (INCMNSZ) in Mexico City, which followed five years of medical school and two years of “social internship” training in which he researched issues that affect medically underserved communities.
It was during his fellowship in geriatric oncology — another specialty Soto brings to the CU Cancer Center — that he traveled to his first annual meeting of the American Society of Clinical Oncologists (ASCO). He made it a point there to meet with Arti Hurria, MD, a pioneer in geriatric oncology, who invited Soto to work with her for a few months at the City of Hope cancer center in California. He returned to INCMNSZ after that and received a Long-Term International Fellowship grant from ASCO’s Conquer Cancer Foundation soon after.
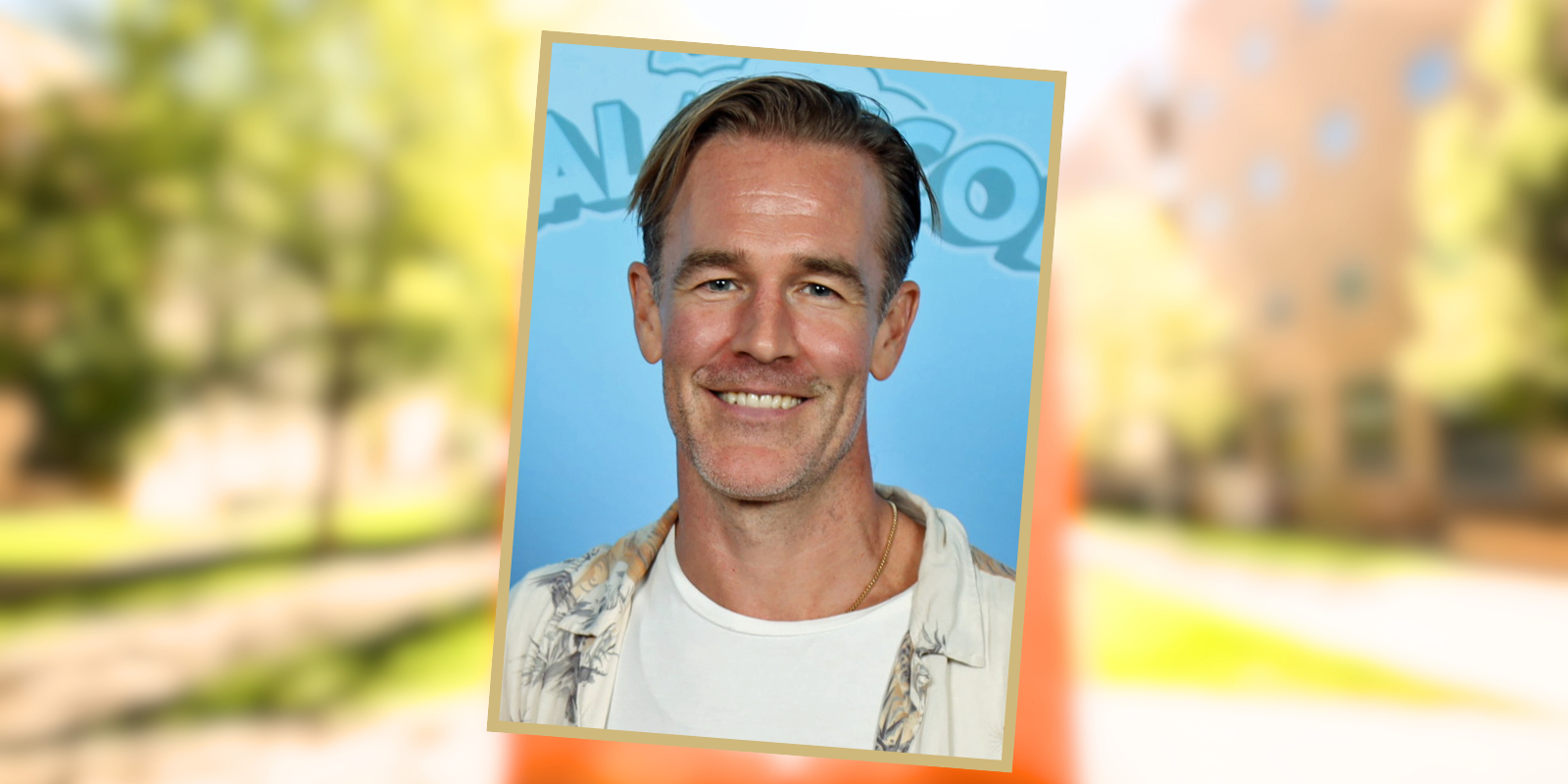
 Enrique Soto Pérez de Celis
Enrique Soto Pérez de Celis
“We already had started a geriatric oncology clinic in Mexico City, but when I came back from City of Hope, we started building it bigger and better,” he says. “We grew our number of patients, we received several national and international research grants for our clinic, and just this past year, we started the first geriatric oncology fellowship in Mexico. It’s a healthy program now, and that’s one of the reasons I said, ‘I can move on. This will continue without me.’”
Wells Messersmith, MD, associate director of clinical services for the CU Cancer Center, says Soto will be a valuable addition to the team as the cancer center looks to expand its global efforts.
“We are so excited to have Dr. Soto joining the CU Cancer Center and the Division of Medical Oncology in the Department of Medicine,” Messersmith says. “He is a highly accomplished researcher in breast, geriatric, and global oncology. He serves as the international oncologist on the board of directors of the American Society of Clinical Oncology, which has 45,000 members; his perspective and experience will be invaluable in his role as associate director for global oncology.”
Cross-cutting connections
Soto says he was drawn to his new role at the CU Cancer Center because it gives him the opportunity to build cross-cutting programs in global oncology and geriatric oncology that could eventually include initiatives for every cancer type. On the global front, he plans to build partnerships with institutions in Latin America, starting with INCMNSZ. He envisions an exchange program that sends U.S. researchers to Mexico and vice versa, and he hopes to create bridges between local communities and global sites to learn more about preventing, diagnosing, and treating cancer in specific ethnicities.
“You can see those connections all across the spectrum,” he says. “Cancer biology and genetics are closely tied.”
In the world of geriatric oncology, meanwhile, Soto is excited to share his expertise in an emerging field that by necessity takes a whole-patient approach to cancer care.
“When we get old, we become very heterogenous, very different,” he says. “If you take 100 people who are all 30 years old, they can pretty much do the same things. If you take their labs, with a few exceptions, they are going to look very similar.
“However, when we age, we all age very differently,” he continues. “You can have 100 people who are 70 or 80 years old or older, and they will have different abilities, different diseases, different tissues, different social problems. One may be fully independent, can run a marathon, drive a car, and another who is the same age and has the same disease, who needs help with their daily chores, has a cane, has fallen, and has many diseases.”
One focus of geriatric oncology, he says, is thinking beyond the disease and beyond the tumor to say, “What does the aging look like in this patient?” That will inform the type of treatment they receive.
Passion for patient care
Working with older patients during his medical training inspired Soto to pursue geriatric oncology as a specialty, and it is the ability to help patients that remains at the heart of the leadership he provides at the CU Cancer Center.
“The antidote to burnout is building strong relationships with your patients, understanding what they really want, what they really value,” he says. “One of the things I like about oncology, and geriatric oncology in particular, is that you get to understand what’s important to the patient, what's important to the family. And in that way, the care you provide is of higher quality. The best part of the job is patients.”
Helping patients was also the reason Soto decided to go into medicine in the first place, choosing it as his career at age 18 before going directly from high school to medical school as is the custom in Mexico.
“It was serendipitous. I thought medicine would be something I could love for the rest of my life, and so far, I’ve been correct,” he says. “We all go through our ups and downs — burnout is a universal thing. But medicine still is a source of happiness for me every day.”