Former Denver Broncos running back Ronnie Hillman, 31, died Wednesday of a rare type of kidney cancer that disproportionately impacts young people who are Black with sickle cell trait or sickle cell disease.
Hillman, who was a 2012 third-round draft pick out of San Diego State University, was the Broncos’ leading rusher in 2015, the season in which the team won Super Bowl 50. He played four seasons with the Broncos before being released by the team in 2016.
On Wednesday, his family announced on Instagram that he had been diagnosed in August with renal medullary carcinoma (RMC), a rare kidney cancer first described in 1995 that primarily affects adolescents and young adults – most patients are diagnosed between ages 11 and 39. Males are affected in 2 to 1 ratio with the disease.
Further, RMC is closely linked with hemoglobinopathies and specifically sickle cell trait and sickle cell disease. Approximately 8% of Americans who are Black have sickle cell trait, so the disease has particularly impacted Black communities.
We spoke with University of Colorado Cancer Center member Nicholas Cost, MD, an associate professor of urology in the CU Department of Surgery and kidney cancer researcher, to learn more about this rare but deadly disease.
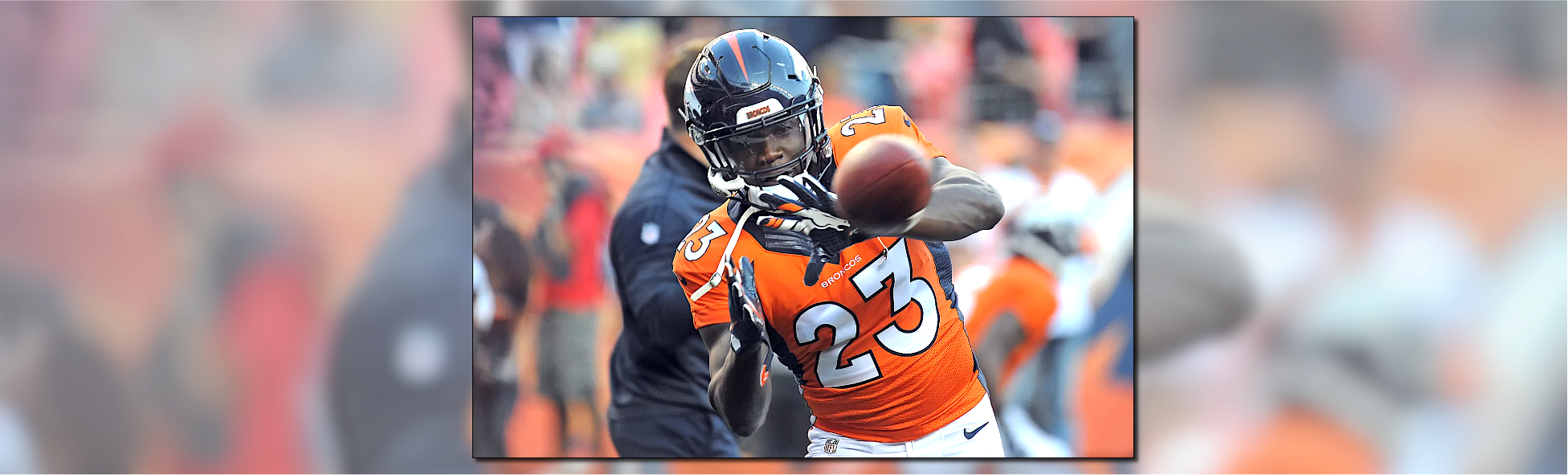
Header image: Steve Nehf/The Denver Post via Getty