Sometimes, getting a caring phone call is just what we need to feel better. And now, research led by a University of Colorado Department of Medicine faculty member shows that a program of scheduled phone calls can significantly improve quality of life for people living with serious chronic illnesses – and that improvement continues for months even after the calls end.David Bekelman, MD, MPH, a professor in the CU Division of General Internal Medicine, led a team conducting a clinical trial of a model program of outpatient palliative telecare aimed at improving quality of life for people with chronic disease. He and his colleagues published their results recently in the Journal of the American Medical Association.
“One really exciting thing about this program is that it’s delivered entirely by telephone,” Bekelman says, “so anybody who’s partially homebound, which is a lot of our target population, or living in rural areas or is just unable to make it to a doctor’s visit can access this.”
306 trial participants
The trial involved 306 adult participants, with a median age of 69, at high risk of hospitalization or death and who reported poor quality of life. The participants were enlisted at the U.S. Department of Veterans Affairs’ Eastern Colorado Health Care System in Aurora, Colorado, and at the Veterans Affairs Puget Sound Health Care System in Seattle, Washington.
VIDEO: David Bekelman, MD, MPH, talks about the results of his clinical trial of a model program of outpatient palliative telecare. Video by CU Anschutz Medical Campus.
Most of the trial participants had chronic obstructive pulmonary disease, or COPD, a group of disorders that cause breathing problems, including emphysema and chronic bronchitis. About 16 million Americans have COPD.
Another 116 participants in the trial had heart failure, including 49 with both heart failure and COPD. And 13 had interstitial lung disease, referring to various diseases that cause scarring of the lungs, making it difficult to breath.
“We’re able to provide great care to people with these conditions through primary care and specialists, and all kinds of disease-specific treatments,” Bekelman says. “Yet a large number of them still have persistent symptoms – shortness of breath, sleep problems, pain, depression, anxiety, fatigue, not enough energy – as outpatients.”
Bekelman and his colleagues wanted to determine if introducing palliative care strategies into routine outpatient care could extend those benefits outside the hospital. And they wanted a model that could be sustainable and transferrable to other settings.
Testing the ADAPT program
The trial measured how a telecare team of a nurse and a social worker – a model program called ADAPT, for Advancing Symptom Alleviation with Palliative Treatment – impacted patients’ quality of life as compared to “usual care,” which for trial purposes included giving the patients an educational handout developed for the study that outlined self-care steps.
“We took a long-standing, successful model of collaborative care delivery that’s been used for depression and adapted it to palliative care,” Bekelman says.
Participants placed in the ADAPT program received six phone calls from a nurse to help with symptom management and another six phone calls from a social worker to provide psychosocial care, over a span of time that averaged 115 days (generally between three and four months).
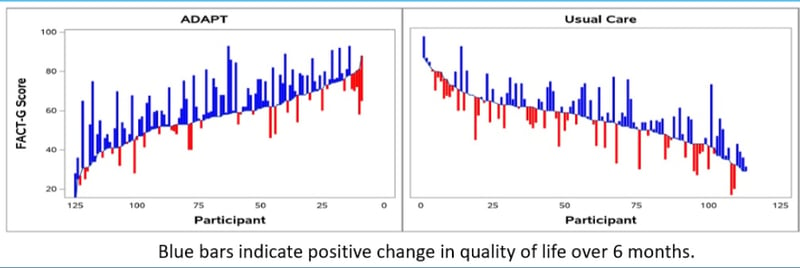 These charts compare change in quality of life for each clinical-trial participant over six months for both the group placed in the ADAPT program and the group receiving usual care, with blue bars indicating a positive change and red bars a negative change. Charts courtesy David Bekelman, MD, MPH.
These charts compare change in quality of life for each clinical-trial participant over six months for both the group placed in the ADAPT program and the group receiving usual care, with blue bars indicating a positive change and red bars a negative change. Charts courtesy David Bekelman, MD, MPH.
Between calls, the nurse and social worker met weekly with a primary care provider and palliative care specialist, and as needed, a pulmonologist and cardiologist. That multidisciplinary team could make care recommendations as needed.
At the start of the program, participants completed a detailed questionnaire designed to measure physical, social, emotional, and functional well-being. They completed the questionnaire again after six months.
Improvement after six months
At six months, participants in the ADAPT group “reported significantly improved quality of life,” Bekelman says. The before-and-after surveys, on a 108-point scale, showed a median increase of six points for the ADAPT group versus a 1.4-point increase for the usual-care group. This difference represents a clinically meaningful change, he says.
“We also found that symptoms of depression and anxiety improved in people that received this intervention,” he says. “Furthermore, we found that among those with heart conditions and lung conditions, their disease-specific health status also had improved at six months.”
“The improvements in quality of life lasted a year, far longer than the phone-care program itself.”
Bekelman and his team hope to collaborate with health systems and possibly insurers on implementing the ADAPT program elsewhere. They’re also discussing additional research into ways to refine the program to make it more feasible for providers with limited resources.
Photo at top: The U.S. Department of Veterans Affairs’ Eastern Colorado Health Care System in Aurora, Colorado, where many of the participants in the clinical trial led by David Bekelman, MD, MPH, were enrolled. Photo by University Communications / CU Anschutz Medical Campus.