There is a tragic, often hidden backstory to asthma that Eileen Wang, MD, MPH, began encountering years ago, even before she went to medical school.
“I worked at a courthouse in Washington, D.C., as an advocate for victims and survivors of intimate partner violence, linking them with services and helping them navigate the legal system,” Wang says. Through her work, she encountered the many “profound impacts” that intimate partner violence can have on victims – injury, fear, financial and housing insecurity, and much more.
“But I also saw a hint of the impact on their health,” Wang says of the survivors she worked with. “There were physical injuries and impacts on mental health, and also increased burden of multiple chronic health conditions, including asthma.”
Wang learned that because the victims she worked with needed to focus on staying safe in the face of abuse, “a lot of them were not able to allocate time and resources to managing their health. And there were many clear cases where the perpetrator was using their health as a power and control tool – impeding their access to medication and medical services.”
That experience, she says, “is where it all started. And so when I went into medicine, I very much wanted to look more at what I had seen – asthma, health inequities, and these key social determinants of health.”
‘What we found was shocking’
According to the U.S. Centers for Disease Control and Prevention, intimate partner violence can include physical and sexual violence as well as emotional and psychological aggression in a current or former romantic relationship.
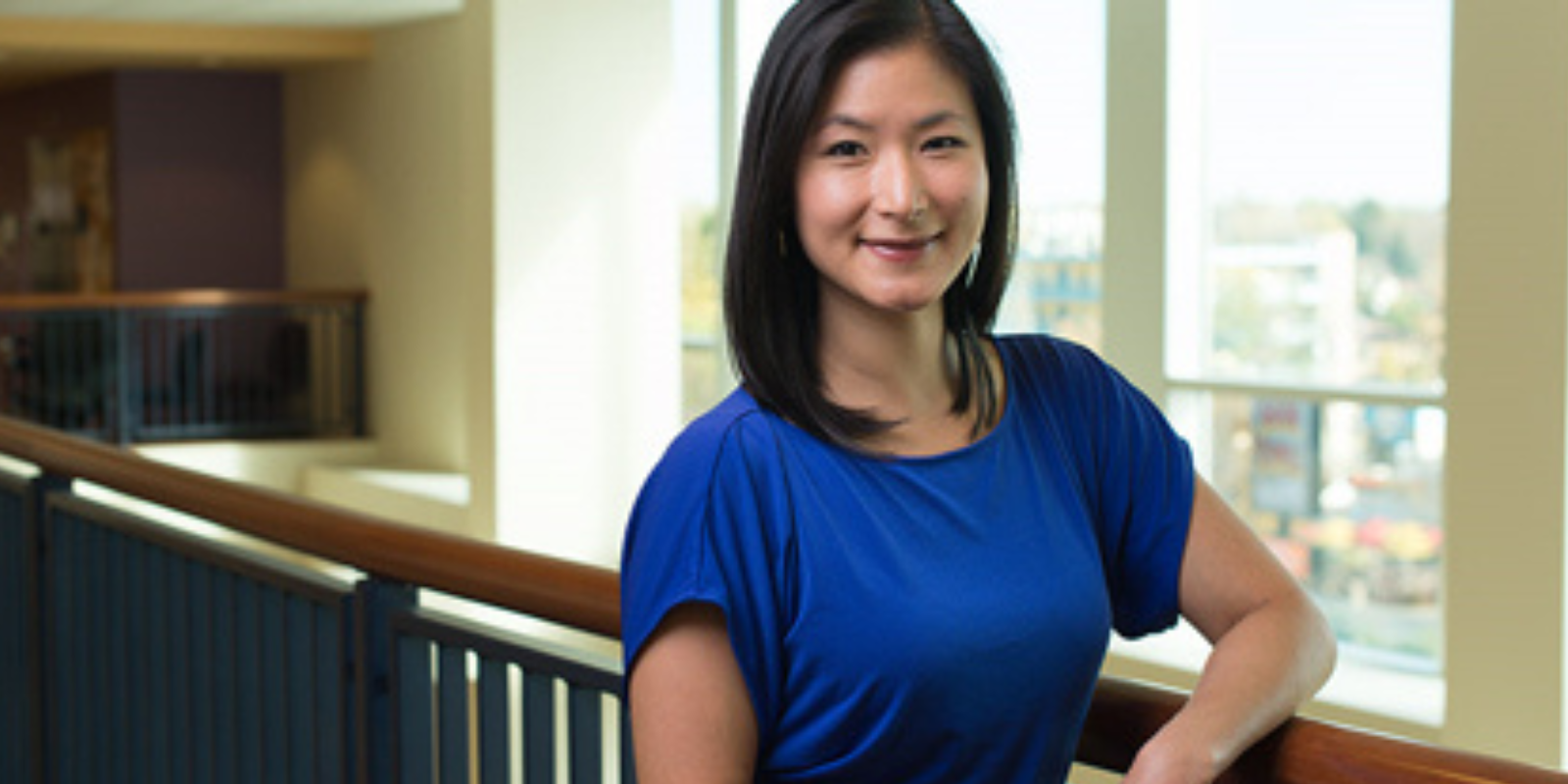
Through years of work, Wang – now an associate professor in the University of Colorado Department of Medicine’s Division of Allergy and Clinical Immunology who practices at National Jewish Health – has established a “pervasive” link between intimate partner violence and uncontrolled asthma.
The startling findings of Wang’s breakthrough 2021 study on the topic, analyzing data on 2,634 adults with active asthma from a U.S. Centers for Disease Control and Prevention survey, drew news media attention.
In that study, she and her colleagues found that 37.4% of the surveyed adults with asthma reported current or past exposure to intimate partner violence – 42.3% of the women and 22.6% of the men. They also found that intimate partner violence was associated with nearly double the odds for asthma exacerbations (also known as attacks or episodes) and more than twice the odds for asthma-related emergency department or urgent care visits as compared to those with no exposure to intimate partner violence.
“It’s a question that hadn’t been asked before through a larger population-based database, and pretty minimally done on a smaller scale,” Wang says. “What we found was shocking to us.”
Even children affected
What was especially surprising, she says, was that the subset of adults with asthma whose exposure to abuse had ended more than 12 months earlier still had higher odds of worse asthma outcomes than those who had never experienced abuse.
“You might assume that someone going through violence currently would have clear impacts on their health,” Wang says. “But even for those who had managed to get out of that situation – whether it was years ago or not – still had a higher risk of worse asthma outcomes. That was very surprising to us.”
The following year, Wang and her colleagues reviewed dozens of previous studies and found more evidence of a link between asthma and intimate partner violence. Further, they found consistent patterns of higher asthma rates among children with a parent exposed to intimate partner violence.
Exploring the why
Which raised the question: Why was this happening?
In recent years, Wang has been working on longitudinal studies – following the same individuals over time – to try to better understand the mechanisms of the link between asthma and intimate partner violence. She’s currently writing a manuscript about the different inflammatory patterns found in patients with asthma with a history of intimate partner violence versus those without that history.
“When we control for important factors – age, race, body mass index, anxiety, depression, chronic stress – none of them fully explains what we’re seeing,” Wang says. “For example, if you treat the related depression, thinking that’ll address the impact on asthma, it seems to be much more complex than that. Intimate partner violence appears to be an important and independent phenomenon that you can’t explain away with these factors. So we’re still investigating.”
‘We all have pivotal roles to play’
While the search for the why and how behind the asthma-abuse link goes on, Wang also remains passionate about the crisis of domestic violence facing society.
Her editorial last year in The Journal of Allergy and Clinical Immunology was titled: “Domestic Violence and Abuse Is Our Issue,” and she challenged clinicians, researchers and their funders, educators, and health care systems to do more to address the issue.
“Domestic violence and abuse is a pervasive global public health issue with a myriad of health sequalae [consequences] that negatively impact all communities,” she wrote, adding: “Clearly, trauma- and violence-informed research and care are critically needed in our field. Therefore, we all have pivotal roles to play.”
Wang recalls a patient who was interested in participating in a study. “But one of the features of the study was that we offered a free Fitbit for people to monitor their activity, sleep, and heart rate. The patient told me they could never wear something around their wrist because of their previous history of abuse when their hands were grabbed; it would be triggering. That was very eye opening, and we changed our protocol.”
Wang adds: “Intimate partner violence is pervasive in our society, and it impacts health and disease. It’s not something we can ignore.”
Photo at top: Courtesy National Jewish Health