As waiting lists continue to grow for patients awaiting organ transplants including heart, liver, lung, and kidney, surgeons are looking for ways to increase the number of organs they can take from deceased donors to use in living recipients.
For many years the gold standard for organ donation was donors whose organs were removed after brain death, meaning blood was still circulating in the body. Recent research, however, has shown that organs removed after circulatory death — or after the heart has stopped pumping blood through the body — are just as viable when it comes to transplant.
Studying two methods
Syed Shahyan Bakhtiyar, MD, MBE, a resident in the University of Colorado Department of Surgery, and Jordan Hoffman MD, MPH, surgical director of heart and lung transplantation, along with a team from the UCHealth Transplant Center, recently published research looking at two methods of procuring organs from donors after circulatory death (DCD) — normothermic regional perfusion (NRP) and super-rapid recovery (SRR) with ex-situ normothermic machine perfusion (NMP). The study was published in March in the American Journal of Transplantation.
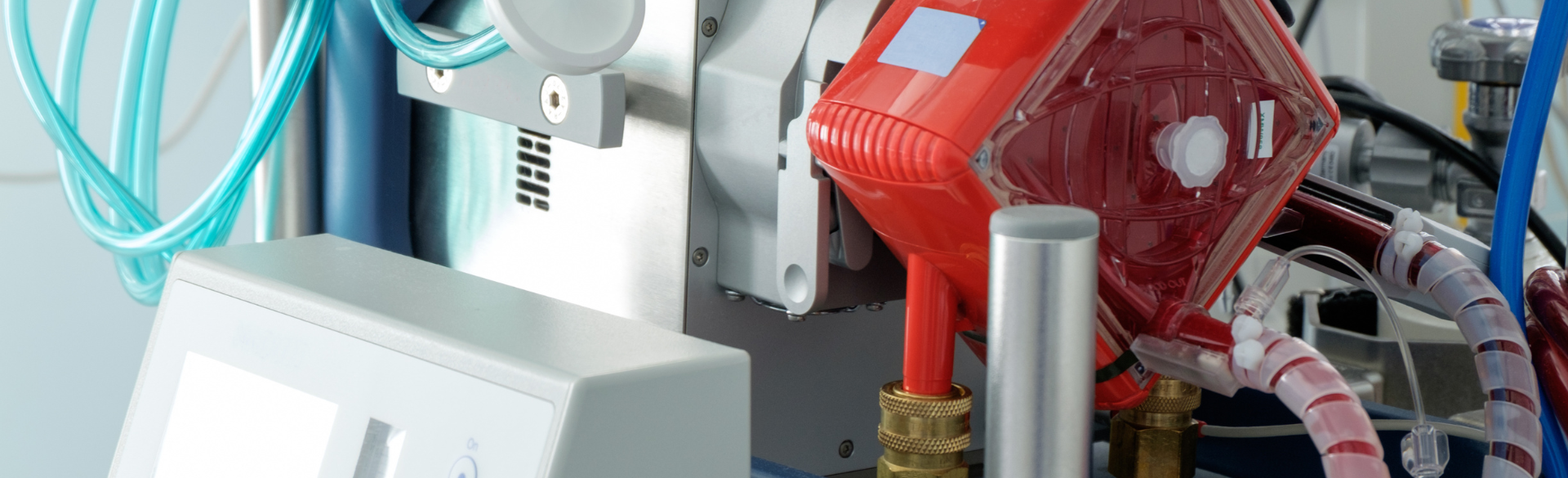
In the former method, a deceased donor is connected to a bypass machine that keeps blood flowing and organs warm; in the latter, organs are removed quickly and put on a machine that perfuses them outside of the body.
For his research, Bakhtiyar looked at the total amount of transplant-viable organs recovered from donors using each method — a number known as organ yield.
“It is crucial to analyze organ yield and cost effectiveness associated with these DCD techniques,” he writes in the paper. “We sought to comprehensively assess the donor allograft yield across various types of procurement. In addition, we aimed to provide a financial structure for the associated costs, with particular focus on NRP donation. We hypothesized that utilization of NRP would yield a superior quantity of viable organs, albeit with higher initial investment. This information could support the decision-making and strategic planning of hospital management and health care professionals seeking to establish DCD programs.”
Cost and other considerations
Chief among the factors Bakhtiyar took into consideration was the cost of super-rapid recovery with ex-situ machine perfusion, a proprietary process that costs between $80,000 and $100,000 per organ. The per-organ cost of NRP, by contrast, was around $2,500.
“We went into the research thinking that logically NRP should be cheaper, because you're essentially perfusing the entire donor with one machine,” he says. “And we assumed we would get more organs because you immediately put the donor on the bypass machine, so you're instantly perfusing organs, and therefore the quality is better, and the surgeons will be more likely to accept these organs.”
There are some advantages to SRR with ex-situ NMP, says Bakhtiyar, who describes the process as “Uber for organs.”
“You can utilize procurement services by the NMP device manufacturers — when you have a donor, they'll send a team, they'll get the organ on their machine and then deliver it to you,” he says. “You don't have to send a surgeon, you don't have to wait for the organ, you can continue your day as is, and the organ will show up.”
The paper includes an opportunity-cost analysis, as well as a recommendation for larger transplant programs to incorporate both procurement techniques into their DCD procurement protocol — NRP for local donors and SSR for out-of-state donors or those at longer distances.
“If the program is really small, and they can't afford to put an entire operating room on hold and send a surgeon, they should just do SRR with ex-situ NMP, because they may not have the luxury of sending a team out,” he says.
Standard terminology and cost analysis
Bakhtiyar says that among the advantages of having the new paper published and being read by transplant surgeons throughout the field is that it begins to standardize terminology for transplants of different organs.
“DCD is such a new thing that in the literature, different people call each technique different things,” he says. “Liver transplant surgeons refer to this technique as SRR with ex-situ NMP, while thoracic surgeons call it DPP, which essentially means the same thing, yet each group employs a different terminology for it. This paper looks at all organs, so we present this uniform, unifying terminology to use. That’s important because if the donor is undergoing NRP, thoracic and abdominal surgeons need to work together.”
Bakhtiyar is also pleased to present information on the cost structure of organ transplantation, including direct and indirect costs. Taken as a whole, he says, the data presented can help programs large and small decide how to best structure their DCD protocols.
“Given our institutional experience as a large DCD program and a large NRP program, I think this paper helps guide other programs that are looking to expand their infrastructure,” he says. “Is NRP the best thing for them, or is SRR the best thing for them? Organ transplantation, for all the benefits that it has, is limited by the amount of available organs. Anything that helps us expand the donor pool is great.”



.png)
