What is a blood clot? How do they form?
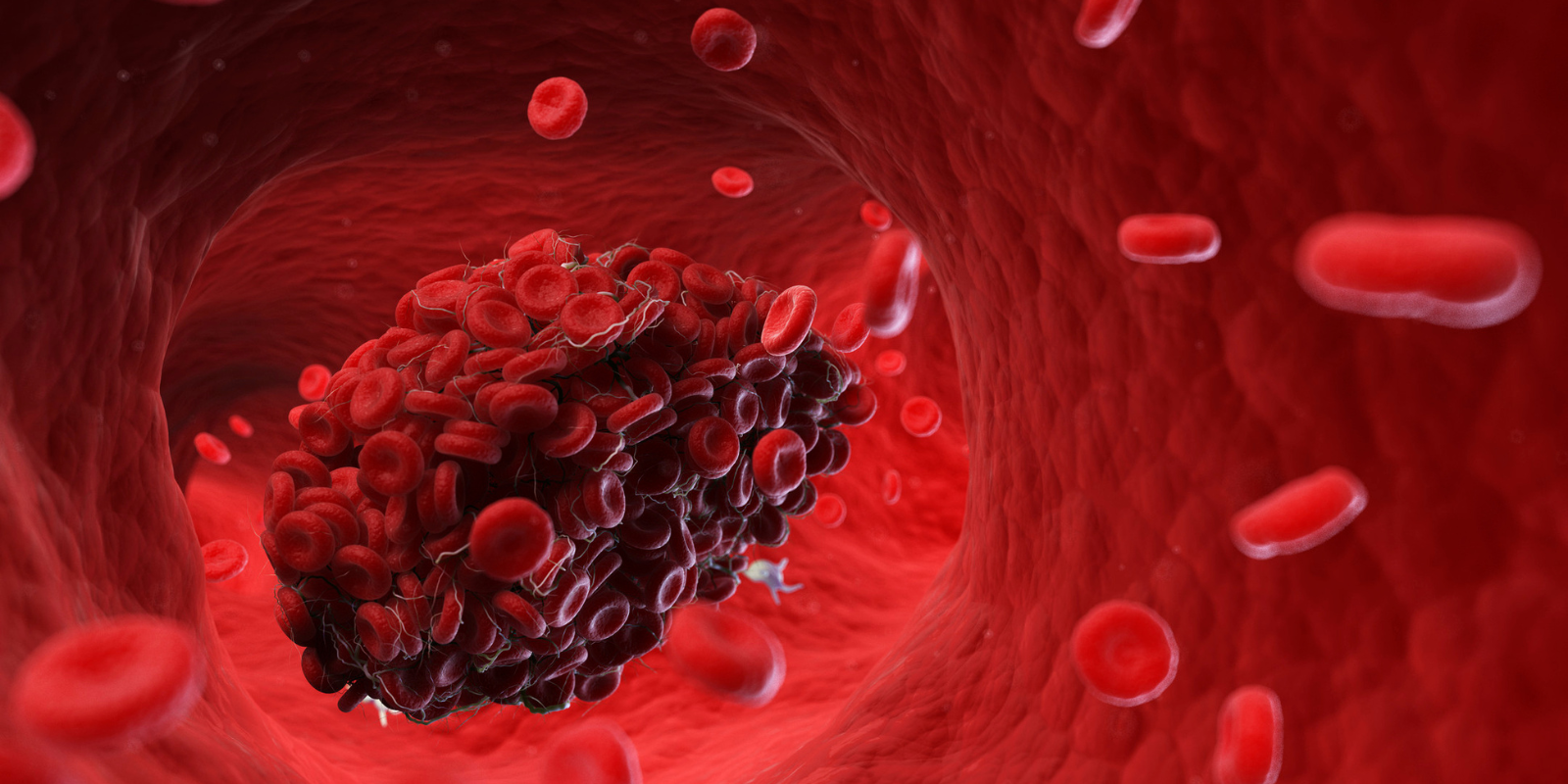
A blood clot is a semi-solid mass of platelets and fibrin that forms in your blood vessels. They can protect you from bleeding too much if you’re injured, but you can develop blood clots for other reasons. Those types of blood clots can cause symptoms and can even be life-threatening.
What are the risk factors for blood clots?
There are three things that happen that increase the risk of blood clots. The first is stasis — a situation where the blood's not moving. We see that in people after surgeries, if they're lying still, or if they have a broken leg that's immobilized.
The second risk factor is a hypercoagulable state, where blood clots more easily. You can have a genetic risk factor that gives you a hypercoagulable state, or it can be caused by a disease. COVID, for example, causes a hypercoagulable state.
The third risk factor is some type of injury to the lining of the blood vessel.
In general, we put blood clots into two categories — provoked and unprovoked. Unprovoked clots happen without an identifiable cause, while provoked clots happen after people have been on a long car ride or a long airplane ride, or they’ve broken their leg, and it's in a cast and immobilized. Those are the ones we can prevent most of the time.
How are those clots prevented?
Outside of occurrences like bad accidents where your leg is immobilized, the best thing is just to get up and move around. If you're on a long car ride or a long plane ride, you want to get up and walk around or stop at an extra rest stop, just to keep the blood circulating through your legs. It’s also important to stay hydrated.
What about compression socks? You always hear about how important those are for long plane rides.
Compression socks help for a couple of reasons. One is that the compression means there is less room for blood to pool. I recommend compression socks not just to prevent blood clots, but also to decrease excessive pooling. If you have a desk job and you're sitting for a long time, or if you're on an airplane, gravity is pulling blood down your legs, so you can get heaviness and pooling and achiness and swelling. Compression socks help that, because they don't allow you to accumulate any extra fluid in your legs.
Why are blood clots dangerous?
The most common place for blood clots to form is in the legs. And the reason to treat them is twofold. One is symptom improvement. If you have a big blood clot, it's like bad traffic and the main highway is clogged. There are some side roads, but you can't get around the accident very quickly, and so you get swelling and heaviness. So one reason to treat it is because the quicker we treat it, and usually that's with blood thinners, the more quickly the clot will break down, and those symptoms will improve.
The real risk is that a piece of the clot could break off and go to the heart and lungs. If it's a big enough blood clot and it goes to the blood vessels in your heart, that can block blood flow into your lungs. That's what we call a massive pulmonary embolism, or PE. If it's a large one, it can affect your ability to breathe, and it can also hurt your heart and your heart's ability to pump blood.
How is a pulmonary embolism treated? Do people notice the symptoms right away?
Some people have very small pulmonary embolisms, and they may not notice them, because it's just going to one very small section of the lungs. But when people have more moderate or substantial amounts of clot, they usually notice, and it's very acute onset. It goes to the lungs, and they feel shortness of breath, chest pain, their heart rate is elevated. Those can be treated in a variety of ways, depending on the severity. If their blood pressure is OK and their heart rate is OK, we just give them blood thinners. But in severe cases, where people have a massive PE that's really impacting blood flow to the lungs and the heart, we can either give them a clot-busting medication, similar to what we give when people have strokes, or there is a procedure called a thrombectomy where we can go in and try to remove part, if not all of the blood clot from the lungs.
What kind of surgeon would do that procedure?
Depending on where in the country you are, those procedures are done either by interventional radiologists, vascular surgeons, or cardiac surgeons. It just depends on the practice.
What are the symptoms of a blood clot?
The most common symptom is significant acute onset swelling. The blood is backing up, so that causes a lot of swelling. People will describe achiness and cramping in their calf muscle or tenderness in their calf muscle as well. But most people come in because they notice that one leg is more swollen than the other. It feels heavy and stiff, and the swelling goes all the way down to the feet.
What is the risk of blood clots after surgery? How is that risk typically mitigated?
Surgery puts you at higher risk for a blood clot for two reasons. For one, most people are sitting around more after surgery. They might be on bed rest because they had a big operation, so they're not moving around as much. Surgery is also a trauma to the body that often puts people into a transient hypercoagulable state where their blood clots more easily. That's why, in the hospital, people routinely have things on their legs called sequential compression devices, or SCDS, which are little pumps that massage the calves. They do the job your calf muscle normally does, helping to circulate the blood through the veins.
We also often put people on low-dose blood thinners after surgery. There's a lot of data that shows that in higher-risk patients, that can decrease the chance that they develop a blood clot.
What is the most important thing for people to know about blood clots?
The biggest thing is not to disregard any symptoms. If people have acute onset shortness of breath or chest pain with breathing, or they notice acute leg swelling, there are a lot of avenues to get an ultrasound and early diagnosis. Getting on blood thinners early helps prevent long term consequences and the risk of it turning into something more serious.




.png)
.png)