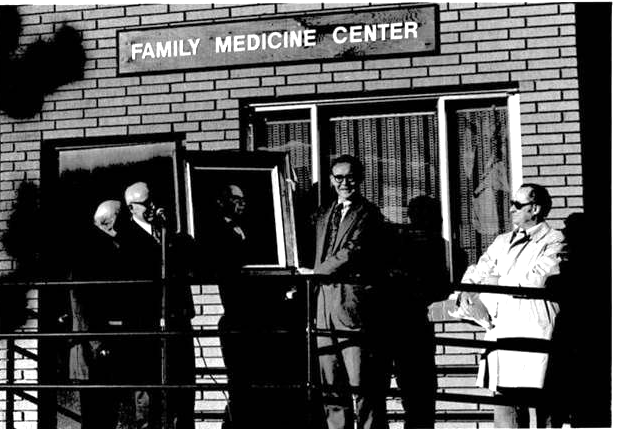
1960s - Dedication of the Department of Family Medicine's first official home on Clermont Street in Denver. (Pictured left to right: Paul E. Woodward, MD; Herbert R. Brettell, MD; portrait of Alfred Frederick Williams, MD; and Harry P. Ward, MD.)
This year, the University of Colorado Anschutz Department of Family Medicine (DFM) proudly celebrates 50 years as an official department, established formally in 1975. Yet our roots reach even deeper—back to 1947, when the foundation was laid for the legacy we celebrate today.
Over the decades, our name has evolved, from “General Practice” to “Family Practice” to “Family Medicine,” but our mission has remained constant: delivering comprehensive, compassionate care for patients and their families across every stage of life.
Today, under the leadership of Chair Myra Muramoto, MD, MPH, FAAFP, we look forward to building on this rich legacy as we continue to grow and innovate for the future.
“I am excited about how well our Department is rising to meet the challenges of our time—challenges brought about by the rapid changes in our own medical school and health system, the healthcare industry and academic medicine at large, and then the world around us. Our Department and our people are simply incredible—we shine! And our home institutions have a growing recognition and appreciation of our Department’s excellence in education, research and clinical care, and how much we contribute to our institutions’ strategic goals.
Change is not always easy, but our faculty, staff, and learners are adapting to major challenges with resilience, creativity, and determination. We are adapting and finding new and better ways to advance our Department’s mission to Heal, Teach, Discover, and Connect. Together.”
From Humble Beginnings to Formal Recognition
The Department of Family Medicine’s journey began in 1947 in the Graduate Education Office, where the groundwork for a new approach to medical training was laid. Just a year later, Frode Jensen, MD, expanded this foundation and launched the General Practice Residency—an innovative move for its time. Over the next two decades, leadership passed through the capable hands of Charley Smyth, MD, and C. Wesley Eisele, MD, who helped shape the residency into a respected program. Among its graduates was Eugene S. Farley, Jr., MD, who would later return as Chair in 1979.
In 1969, a pivotal moment arrived as Family Medicine emerged as the 20th distinct medical specialty. The residency was transformed into one of the first thirteen Family Medicine programs in the country, and “the Division of Family Practice” was established within the Department of Internal Medicine, led by internist Herbert R. Brettell, MD. Then, in 1975, with a push from the Colorado Legislature, the division stepped into its own identity as the “Department of Family Medicine,” with Dr. Brettell becoming its first chair.
Supporters and Milestones
Shortly after, a major supporter and catalyst for the Department’s growth stepped in, the Rose Medical Center (originally Rose Hospital and later Health One operation), who hosted the Department’s first University of Colorado Family Medicine Residency Program. Support from the Rose Medical Center sparked the education and care shaping the Department today.
Just two years later, and only a short distance from Rose Medical Center, the A.F. Williams Family Foundation generously donated a building on Clermont Street for the Department to use as both a clinic and administrative headquarters. Today, that building is home to the A.F. Williams Family Medicine Center—a vibrant hub that welcomes countless residents and draws aspiring physicians from across the country.
By the early 1980s, the Department became fully integrated into the CU Anschutz educational mission and joined the faculty practice plan. During this time, the Department pioneered the nation’s first primary care practice-based research network, the Ambulatory Sentinel Practice Network (ASPN), launched from the Clermont building under Dr. Gene Farley’s leadership. Building on innovations such as the Family Medicine Information System—which managed billing, documentation, patient data for all Colorado residencies and 27 practices well before desktop computers existed—and on collaborations like Dartmouth’s COOP, these efforts secured major funding and ignited the practice-based research network movement, which is now a global model.
During the 1990s, the Department launched residency programs at Swedish and University Hospitals, introduced an urban training track at Denver Health, and formally embraced research as a core priority. Another notable advancement was the creation of a Family Medicine Scholars Program which laid the groundwork for mentored scholarly activities for all medical students.
Today, with innovation clearly in our DNA, the Department continues to grow and flourish and has consistently been in the top ten national ranking for twenty years (when Family Medicine was a specific category. See Dr. DeGruy below). Although this is not a comprehensive list of all the Department’s milestones and major accomplishments, it is a small glimpse into the admirable and extensive history of the DFM.
50 Years of Leadership
The Department’s evolution has been shaped by a legacy of thoughtful leadership, starting with its inaugural Chair, Dr. Brettell, in 1975. Three years later, R. Neal Chisholm, MD—the first family physician to join the regular faculty at the CU Anschutz School of Medicine, followed. Leadership shifted to Dr. Farley in 1979, whose impact continues today through the Farley Health Policy Center. Dr. Chisholm returned briefly in 1983 before Larry Green, MD, took the helm in 1985, leading the Department through a period of remarkable growth. During Dr. Green’s 1991 sabbatical in Europe and South Africa, Donald C. Iverson, PhD, served as acting chair.
In 1999, Frank V. deGruy III, MD, MSFM, stepped in, serving for over two decades—the longest tenure of any Chair to date. He was succeeded in 2021 by acting Chair Colleen Conry, MD, and then by the current Chair, Dr. Muramoto, who leads the Department today. Together, these leaders have shaped a rich legacy, rooted in clinical excellence, education, and policy innovation. A tradition made possible through the hard work of the faculty, staff, and learners who pass through our doors year after year.
Reflections on the Department’s Anniversary
As the Department celebrates 50 years as an official department, we invited Dr. Muramoto, our current Chair, along with former Chairs Dr. deGruy and Dr. Green, to share their reflections on this milestone.
 Myra Muramoto, MD, MPH, FAAFP: Woodward-Chisholm Professor and Chair for the University of Colorado Department of Family Medicine.
Myra Muramoto, MD, MPH, FAAFP: Woodward-Chisholm Professor and Chair for the University of Colorado Department of Family Medicine.
- When you became chair in 2021, what was your vision for the Department and how has that vision evolved over the past five years?
“The CU Anschutz Department of Family Medicine has long been a source of inspiration in the field of Family Medicine for the excellence, depth, and breadth of its many programs. My vision was to build on our Department’s existing strengths and foster greater integration and synergy between mission areas and the program silos that naturally develop in a large department. I also envisioned strategically focusing and growing in areas I saw as untapped opportunities. These opportunities included engaging in more clinical trial research, nurturing growth in strategic research focus areas, and partnering with the Aurora Wellness Community to help realize the vision of a biopsychosocial, wrap-around approach to improving health for our neighboring underserved populations.
I aimed to build the infrastructure for the broad spectrum of practice-based translational research: from early-stage work in our innovation practice, to mid-stage practice-based research in the Colorado Ambulatory Partnership for Health Innovation and Research Excellence (CAMPHIRE) statewide network of primary care practices, and through late-stage efforts of turning research evidence into health policy through the Farley Health Policy Center. Even with unexpected hiccups along the way, my original vision has remained fairly constant. I am grateful that much of that vision is now coming to fruition.”
- How is the Department adapting to the evolving landscape of Family Medicine — in education, research, or patient care?
“Healthcare continues to rapidly evolve, and academic medicine faces new challenges in sustaining and growing its tri-partite mission. To thrive, the DFM is adapting in multiple ways to advance our mission in patient care, education, and research.
In July, we opened our Centerfield “Innovation Practice,” a “laboratory” to develop and test new ways to deliver patient-centered and relationship-based primary care. This space also allows us to partner with other innovators in patient care technology, care delivery models, and primary care team composition. We also opened the Aurora Wellness Community Health Center (AWCHC), which is the primary care clinic anchor for the CU School of Medicine’s Aurora Wellness Community initiative. Designed to assemble a wrap-around approach to health for the disadvantaged and underserved neighborhoods surrounding our campus.
Chronic pain is a vexing problem for both patients and primary care practices. To better support primary care providers in caring for these chronic pain patients, we launched the Whole Person Pain Service (WPPS). This is a behavioral health forward, telemedicine-only service providing care to patients with chronic pain on chronic opioid therapy. This program partners with their primary care provider to ensure consistent, evidence-based, and interdisciplinary care with an emphasis on both pain psychology interventions and medication management.
In research, we have formed an exciting new collaboration—the Colorado Ambulatory Partnership for Health Innovation and Research Excellence (CAMPHIRE), a merging of the Practice Innovation Program (PIP) and the State Networks of Colorado Ambulatory Practices & Partners (SNOCAP). CAMPHIRE is an integrated partnership of innovators, scientists, and clinicians who produce and translate evidence in ambulatory care and community settings. CAMPHIRE collaborates with practices, partners, and communities to conduct and promote research, education, and innovation in real-world clinical settings. Our goal is to foster collaborative practice and community-based initiatives that improve health and well-being across the lifespan.
In education, our Rural Program received state funding for the Colorado Rural Healthcare Workforce Initiative which builds on its 20-year history of medical student education to support creation of “rural tracks” for other healthcare disciplines. The Rural Program’s successful model of longitudinal clinical education model is now in 15 Colorado public schools training physicians, dentists, nurses, physician assistants, public health and behavioral health professionals.
Addiction Medicine and Hospice and Palliative Medicine (HPM) physicians are both specialties with significant physician workforce shortages. Prevalence of substance use disorders is often higher in rural communities than urban communities, yet rural residents lack access to treatment. To help address this need, our Addiction Medicine Fellowship received a HRSA grant to expand the fellowship with a rural training track. As the US population ages and also becomes more aware of the benefits of hospice and palliative care, there is a growing demand for these physicians. Our HPM fellowship developed an innovative ACGME accredited community-based fellowship which provides opportunity for up to 25 physicians to complete HPM training in their home communities, rather than relocate for a traditionally structured fellowship. Our Family Medicine Residency launched its Longitudinal Leadership Concentration to prepare graduates with further leadership skills to become confident and effective leaders and change agents in the healthcare and community settings in which they serve.”
 Frank V. deGruy III, MD, MSFM: Woodward-Chisholm Professor and Chair for the University of Colorado Department of Family Medicine.
Frank V. deGruy III, MD, MSFM: Woodward-Chisholm Professor and Chair for the University of Colorado Department of Family Medicine.
- What are you most proud of in terms of the Department’s evolution and your time as Chair?
“The creation of the Rural Program in the Department and in the School of Medicine. With support from Dean Richard Krugman, MD, we moved the Colorado Area Health Education Center (AHEC) program into the DFM. The creation of a rural track in the medical school curriculum, established an endowed deanship for rural health, and greatly augmented rural research through the High Plains Research Network and PeachNet.
- Expanded the research portfolio. Our consortium of Practice-Based Research Network (PBRNs) led this effort. For several years we directed the AHRQ-funded national PBRN consortium, but research across many domains flourished. Extramural grant funding expanded 15-fold.
- Our faculty have directed the American Academy of Family Physicians (AAFP’s) National Research Network. Our researchers have won over $100M in grant awards. Our faculty have served as President of NAPCRG, the leading international primary care research organization.
- Introduced Integrated Care into the fabric of the Department. In 1999 there were only three departments practicing the integration of behavioral health into primary care; we led a national movement toward integrated care that now includes literally thousands of practices, hundreds of residency programs, scores of departments, and the formation and leadership of AHRQ’s Integration Academy. Some of our faculty have served as president of the Collaborative Family Healthcare Association (CFHA), a 1000-member organization of integrated practices and programs.
- Overall growth of the Department, from 74 faculty, one residency program, and one clinic to a maximum of 300 regular faculty, 700 clinical faculty, three residency programs. Including one rural track, one urban underserved track, fellowships in palliative care, sports medicine, and primary care research, a large research portfolio, and [multiple] clinics. (We subsequently trimmed back some of these programs.) The department has consistently been top ten national ranking for twenty years.”
- How do you think the Department has shaped the broader field of Family Medicine — locally and nationally?
“High-profile leadership across clinical, educational, research, and organizational domains:
- Faculty have served as chairs and board members of major national organizations, including the American Board of Family Medicine (ABFM) and the American Board of Medical Specialties (ABMS).
- Department leaders have held presidential roles, leadership roles, and delegate roles in key professional associations such as the American Academy of Family Physicians (AAFP), the Association of Family Medicine Residency Directors (AFMRD), the Society of Teachers of Family Medicine (STFM), the Association of Departments of Family Medicine (ADFM), the North American Primary Care Research Group (NAPCRG), and the Collaborative Family Healthcare Association (CFHA).
- The Department has maintained leadership roles in virtually every major Family Medicine organization, as well as international Family Medicine bodies and numerous national medical organizations.
The Department has provided consultation and guidance to Family Medicine programs across the country, with recommendations often modeled on innovative approaches to care, education, and research developed—and successfully implemented—here in this Department. Additionally, the Department has entertained scores of visitors seeking insight and advice about our programs.”
 Larry Green, MD. Distinguished Professor and Epperson Zorn Chair for Innovation for the University of Colorado Family Medicine and Primary Care.
Larry Green, MD. Distinguished Professor and Epperson Zorn Chair for Innovation for the University of Colorado Family Medicine and Primary Care.
- What were some of the biggest challenges the Department faced during your time as Chair, especially in the early years, and how did those experiences help shape what it has become today?
“The challenges I faced derived from the origin story of Family Medicine and initial development efforts in the 1970's of the new specialty. Family Medicine was born at a time of societal disruption and emerged as a desperately needed corrective action to the decline of general practice—not a knowledge or technology breakthrough. Most people knew family doctors, and they wanted them, and legislatures and community hospitals embraced Family Medicine. Family Medicine committed to replacing general practitioners with purposefully well-prepared family physicians able to serve any community as a personal physician and assure primary care for all.
Contemporaneously, there were also great public expectations of medicine rising to cure diseases with powerful new, highly specialized knowledge and technology in expanding academic health centers. Family Medicine represented a counter-cultural movement to specialization, reductionism, and a commitment to biomedicine, claiming instead a focus on the whole person in the context of family and community rather than a type of problem or an organ. Family Medicine as a specialty aimed to advance generalism, primary care, and personal doctoring. This lack of alignment of Family Medicine’s interests and commitments resulted in academic centers not placing a high priority on the development of the new specialty. Despite the history of its general practice program, the University of Colorado Anschutz School of Medicine was not particularly welcoming to Family Medicine, whereas the state of Colorado was enthusiastic about Family Medicine. Rapid expansion of Family Medicine residencies occurred in the 1970's, mostly anchored in Colorado communities, while efforts to develop Family Medicine at the medical school as an academic enterprise proceeded much more slowly, its vision not embraced by the medical school. The Department was not thriving until 1984. This situation determined the tasks of leadership: explain and defend Family Medicine; sustain partnership with the state and Colorado communities and especially Rose Hospital; seize and grow willing university partnerships; align with an evolving university-based multispecialty practice; build educational and research infrastructures; support and learn from national Family Medicine organizations.”
What values or lessons from the Department’s founding were passed down to you by your predecessors, and how did they shape your leadership?
“Personal physicians have been created in some form by all known human societies. A family physician is a generalist and a personal physician. Primary care is the foundation of successful, affordable health care systems and a natural home base for family physicians. Generalism is an exciting way of being, knowing, and doing that is a necessary complement to specialism in human systems, including health care systems. Being a family doctor is a calling as well as a role—not just another job. There is much to be discovered in family practice and primary care that can help people be healthier. Family Medicine has a duty to serve the public first and foremost. Family Medicine has a duty to increase the knowledge base of medicine and constantly improve the practice of family physicians.”
Thank you to Dr. Muramoto, Dr. deGruy, and Dr. Green for their guidance and insight as we celebrate this special anniversary. The work happening in every corner of the Department began with a simple but important idea: caring for patients and their families—a legacy each of us helps to carry forward to the next generation of physicians, researchers, educators, and learners.

1949- Charley Smyth, MD. Director, the General Practice Residency.


1969 - Herbert R. Brettell, MD Head, Division of Family Practice. 1975 - Chair of the newly made Department of Family Medicine.

1978 - R. Neal Chisholm, MD. Acting Chair. 1983 – Acting Chair.

1979 - Eugene S. Farley, Jr., MD. Chair. General Practice Residency Graduate. Inspiration behind the Farley Health Policy Center

1985 - Larry Green, MD. Chair.

1991 - Donald C. Iverson, PhD. Acting Chair.


2021 – Colleen Conry, MD. Acting Chair.

2021 – Myra Muramoto, MD, MPH, FAAFP. Current Chair.
Resources: Overview of Department of Family Medicine
Special thanks to Dr. Larry Green and Linda Niebauer for their help with the Department's history.
.png)
.png)