When Dennis Roop, PhD, joined the University of Colorado School of Medicine to lead the Gates Program for Stem Cell Research in 2007, the first postdoc he recruited was Ganna (Anya) Bilousova, PhD, a Ukrainian researcher who had recently completed graduate training in biochemistry at CU.
Only a year before, Japanese researcher Shinya Yamanaka, MD, PhD, had created a sensation in the scientific community when he reported that he could reprogram adult skin cells into embryonic-like cells, introducing the world to induced pluripotent stem cell (iPSC) technology. When stem cells are pluripotent, they can develop into any number of cell types in the body.
But early iPSC technology wasn’t simple. The process was time-consuming and resulted in very few viable cells, as the efficiency of gene editing is less than 5%.
One of Bilousova’s first projects in Roop’s lab in the Department of Dermatology was to determine whether Yamanaka’s iPSC research was reproducible, and if so, whether it could be improved upon. The answers were yes and yes.
‘We need a molecular biologist’
Although Bilousova was new to dermatology and inexperienced with keratinocytes – the primary cells of the epidermis -- she quickly impressed Roop with her creative problem solving in the lab.
“I call Anya a cell whisperer because she has this innate ability to look at cells when they're growing in a petri dish and just knows what they need to be happy,” Roop quipped, and he’s only half-joking.
Having established that Yamanaka’s research was robust and reproducible, Bilousova turned her focus to improving the iPSC technology to yield real-world applications in dermatology.
“Anya came to me and said, ‘You know, we need a molecular biologist, and I just happen to know somebody,” Roop recalled.
That somebody was Bilousova’s husband, Igor Kogut, PhD, who had also emigrated from Ukraine to obtain his PhD at CU – in biochemistry and molecular genetics. With Bilousova’s expertise in cell biology and Kogut’s background in molecular genetics, they made a formidable team. Roop provided guidance throughout as well as support navigating grant applications.
Since then, Bilousova and Kogut established their own independent research laboratories but continued their close collaboration with Dr. Roop on developing therapies using iPSCs. Kogut is now assistant professor of dermatology and Bilousova is associate professor of dermatology.
From concept to cures
Growing genetically modified human skin in a lab may have sounded like science fiction a few years ago, but recent strides are making iPSC technology a reality. Bilousova’s and Kogut’s work in collaboration with Roop could offer hope for a better quality of life for patients with devastating skin-blistering diseases, such as epidermolysis bullosa (EB). Not only that, it could open the door to cures for other diseases.
“These embryonic cells can be expanded upon indefinitely,” said Bilousova. “And as a result, we can do a lot of things with them.”
Including precise gene editing to correct the mutation that causes EB.
With the assistance of their laboratory members, Bilousova and Kogut found ways to speed up the process and make more cells viable. In late 2022 and early 2023, they patented two new technologies – the result of more than a decade of work.
“One is a high-efficiency RNA-based reprogramming, which is a protocol that allows us to reprogram at least 80% of the cells we plate,” said Bilousova. “The second patent allowed us to combine this high-efficiency reprogramming method with gene editing. And that allows us to shorten the procedure for the generation of genetically corrected iPS cells that we can use for the treatment of inherited skin-blistering diseases.”
The higher success rate makes the process more practical for clinical applications. Because skin has been generated “in a dish” for many years now, techniques are already available that allow for functional skin to be transplanted back to patients. In addition, the researchers are investigating a promising alternative involving a form of “spray-on skin” that could improve upon current skin graft techniques.
The numerous grants they’ve received, from entities like the National Institutes of Health and Department of Defense, are testament to the potential real-world applications of their work.
Moving from lab to clinical trials
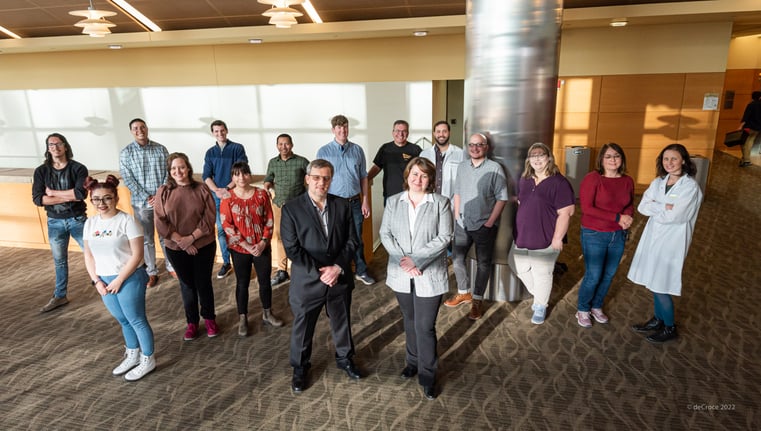
Igor Kogut, PhD, and Anya Bilousova, PhD, with the support of their lab teams, have developed patented technology to produce induced pluripotent stem cells (iPSCs), which will be manufactured at Gates Biomanufacturing Facility for use in clinical trials. |
Roop, Bilousova and Kogut were recently awarded funding from the Epidermolysis Bullosa iPS Cell Consortium to manufacture their stem-cell created skin grafts. They’ve begun moving their technologies into the Gates Biomanufacturing Facility (GBF) to launch the production of their modified mRNA protocol.
“It seems like they were able to successfully produce the molecules,” Bilousova said. “We recently tested them in our lab and they performed as expected, so we believe it’s going to work.”
Their next step is to move the combined gene editing and reprogramming to the GBF, which will produce clinically relevant, genetically corrected, patient-specific iPS cells, ready for differentiation.
Once the cells are differentiated into skin organoids, they are ready to use on patients for clinical trials. Which is again where the GBF comes in.
“The Gates Biomanufacturing Facility will help us make the whole complex protocol suitable for clinical manufacturing,” said Bilousova. “And once we accomplish that, we can go to the FDA and ask permission to initiate a clinical trial to treat the patients.”
The researchers are cautiously optimistic, recognizing there’s still a lot of work to be done.
“It's pretty cool to be at the forefront of the whole technology and make a difference for the quality of life of these patients,” said Bilousova.
Kogut says many diseases could benefit from this technology, including inherited hematological diseases like Fanconi anemia.
“We could be providing a cure for currently incurable diseases,” he said. “We’re really in the position to help people.”
Note: Toni Lapp contributed to this article.

-2.png)

%20for%20children%20and%20young%20adults%20with%20relapsed%20or%20refractory%20solid%20tumors.%E2%80%9D%20(1)-1.png)