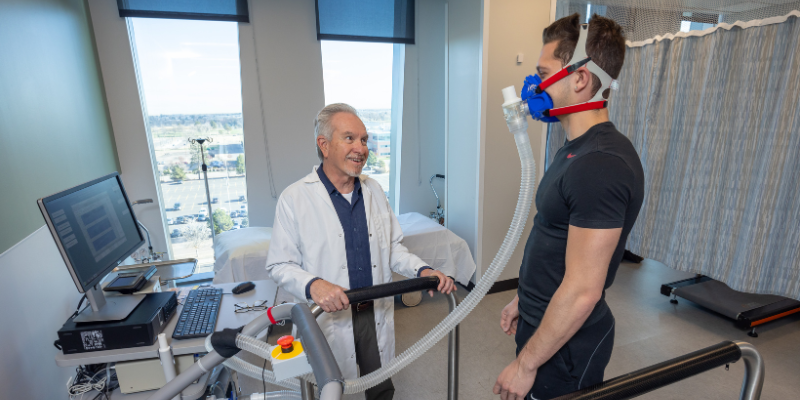
A leader in endocrinology as well as obesity research and clinical care, Dr. Dan Bessesen has spent more than three decades studying the complex mechanisms of weight regulation and metabolic health. As a Professor of Medicine at the University of Colorado School of Medicine (CU-SOM) and the Executive Director of the CU Anschutz Health and Wellness Center (AHWC), Dr. Bessesen has committed himself to research, education and clinical practice in the fight against obesity.
Dr. Bessesen grew up in the mountains of Colorado where his father was the only physician in Summit County before the construction of Interstate 70 and the Dillon Reservoir. He graduated from Colorado State University where he was selected as a member of the United States International Traveling Debate Team following his senior year. He was an AOA graduate of the CU-SOM and went on to do his internal medicine residency and chief residency at CU. After working as a primary care physician at the Eastside Clinic affiliated with Denver Health (DHHA), he completed an endocrinology fellowship under the research mentorship of Dr. Robert Eckel. He then started his own laboratory at DH where he has worked clinically for the past 32 years. Dr. Bessesen served as the Head of the Section of Endocrinology for 20 years prior to becoming the Director at the AHWC in 2019. Dr. Bessesen has been listed by 5280 magazine as one of the top endocrinologists in Denver 18 times over the last 21 years.
Dr. Bessesen’s early research studies focused on nutrient sensing by the brain in animal models of obesity and how the movement of dietary fat between tissues including skeletal muscle, liver, and adipose tissue contributes to the development of obesity. Those initial studies were conducted on animals that were either prone to or resistant to obesity-prompted studies in human subjects who are naturally thin. These studies did not show any evidence that naturally thin people had higher metabolic rates or responded to overeating by burning extra calories. Rather, the studies showed that naturally thin people’s brains sensed positive energy balance more accurately than those of people prone to weight gain. In addition, naturally thin people appear to metabolize fat differently at night while they sleep as compared to those prone to weight gain, an unexpected finding. Ongoing studies are examining the adaptive responses to weight loss that promote weight regain in people with obesity who have lost weight by diet alone or diet plus exercise.
Along with the clinical trials group at the AHWC, Dr. Bessesen is studying a number of new anti-obesity medications including the combination of semaglutide with the long-acting amylin analogue cagrilintide and the new triple (GLP-1, GIP and glucagon) agonist retatrutide. In preliminary findings from phase 2 trials, these medications appear to be even more effective than currently available highly effective anti-obesity medications. Dr. Bessesen noted that there are over 100 medications in the anti-obesity pipeline. While not all of these medications will become commercially available, overcoming years of production problems and high costs will give way to broader accessibility of highly effective medications to treat obesity. These therapeutic innovations hold the promise to dramatically change the way clinicians care for a wide range of health problems from diabetes to fatty liver disease, heart disease, and potentially even cancer.
D r. Bessesen has also conducted studies of obesity treatment in primary care settings. In one study funded by the Patient-Centered Outcomes Research Institute (PCORI), a ‘toolbox’ approach to weight management was tested in a medically underserved population. This study showed that while patients with obesity initially favored lifestyle approaches to weight management, over time they and their clinicians tended to move towards the use of anti-obesity medications which had higher levels of effectiveness. He was also involved in a study using data from electronic medical records to examine weight management practices in 2.2 million adults in eight large healthcare organizations. These studies showed that less than 5% of people living with obesity, who are eligible to use an antiobesity medication, ever receive a prescription for one. This study showed that a small portion of physicians is responsible for a large majority of the prescriptions for antiobesity medications reflecting discomfort on the part of many physicians to treat obesity as a medical condition in an effort to advance the clinical practice of obesity medicine, In response to this reality, Dr. Bessesen has been involved in the development of treatment guidelines for the Endocrine Society and the American Thoracic Society. He has also been actively involved in the Obesity Society, the premier scientific professional society in the area of obesity for which he served as President in 2022. He has co-edited for textbooks on the treatment of obesity.
r. Bessesen has also conducted studies of obesity treatment in primary care settings. In one study funded by the Patient-Centered Outcomes Research Institute (PCORI), a ‘toolbox’ approach to weight management was tested in a medically underserved population. This study showed that while patients with obesity initially favored lifestyle approaches to weight management, over time they and their clinicians tended to move towards the use of anti-obesity medications which had higher levels of effectiveness. He was also involved in a study using data from electronic medical records to examine weight management practices in 2.2 million adults in eight large healthcare organizations. These studies showed that less than 5% of people living with obesity, who are eligible to use an antiobesity medication, ever receive a prescription for one. This study showed that a small portion of physicians is responsible for a large majority of the prescriptions for antiobesity medications reflecting discomfort on the part of many physicians to treat obesity as a medical condition in an effort to advance the clinical practice of obesity medicine, In response to this reality, Dr. Bessesen has been involved in the development of treatment guidelines for the Endocrine Society and the American Thoracic Society. He has also been actively involved in the Obesity Society, the premier scientific professional society in the area of obesity for which he served as President in 2022. He has co-edited for textbooks on the treatment of obesity.
Dr. Bessesen has also been deeply committed to medical education and research mentorship. He directed the medical student nutrition and biochemistry course at the CU-SOM for 14 years, and his dedication to teaching was recognized with both the President’s (1997) and Chancellor’s Award (2018) for teaching excellence as well as the American Society for Nutrition’s Roland L. Weinsier Award for Excellence in Medical/Dental Nutrition Education in 2008. His work mentoring postdoctoral fellows and junior faculty in research was recognized and supported by a K24 grant from the National Institute of Diabetes and Digestive and Kidney Diseases (NIDDK) from 2001-2011. Dr. Bessesen served as either Associate Director or Fellowship Program Director in Endocrinology, Metabolism, and Diabetes from 1991-2019. In 2019 he became the founding Program Director for the Colorado Obesity Medicine Fellowship training program which he continues to lead. He is also the principal investigator on a T32 grant from NIDDK that supports postdoctoral research training in obesity, metabolism and type 2 diabetes.
Dr. Dan Bessesen remains a driving force in understanding and addressing one of the most pressing health issues of our time. His contributions, spanning research, clinical care, and education, continue to shape the future of obesity care.



.png)