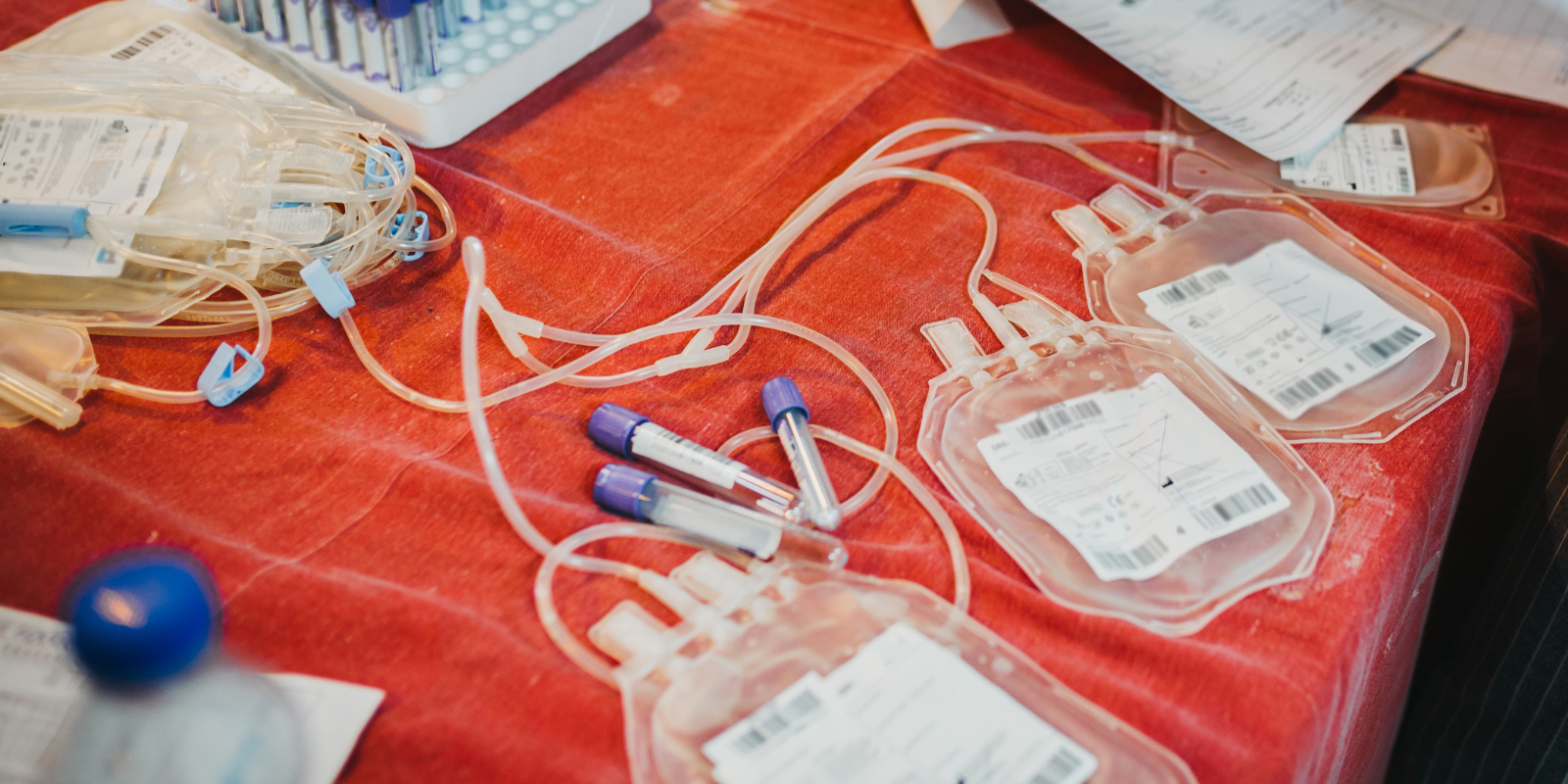
Every year, more than 14 million units (pints) of blood are transfused in the United States. Every two seconds, someone needs blood or blood products. Yet there’s a declining pool of blood donors, and blood products have a limited shelf life.
The American Red Cross declared an emergency blood shortage in July after its national blood inventory plummeted more than 25%. It resorted to offering gift cards to attract donors.
A blood-supply emergency can mean transfusion delays and rationing, endangering patients. Which raises the question: Is synthetic blood a potential answer?
Keith Neeves, PhD, address that question in a lively article entitled, “Where’s the Synthetic Blood?” for the science and technology publication Asimov Press. Neeves is a professor of bioengineering and pediatrics in the University of Colorado School of Medicine and scientific director of its Hemophilia and Thrombosis Center.
“Because of the ubiquity of transfusion for so many things, including surgery, trauma, and cancer, there’s an obvious push to move away from the reliance on human donations,” Neeves says.
Formidable challenges
The issue hits close to home for the Hemophilia and Thrombosis Center, which provides treatment and management of genetic bleeding and clotting disorders to patients from across Colorado and neighboring states.
Blood donations sharply declined during the COVID-19 pandemic, particularly among people age 24 and under, and donation levels have not recovered, he says. And whole blood supplies generally have a shelf life of only 21 to 35 days, the Red Cross says. Red blood cells can last up to 42 days, but platelets – cells that help form clots to stop bleeding and heal wounds – are usable for only about five days.
In the article, Neeves calls the creation of synthetic blood – a catch-all phrase for various blood substitutes – “one of the holy grails of biomedical research as it would alleviate such shortages and overcome current barriers to obtaining and storing blood products.”
But while research has pointed to promising ways to create synthetic blood, there are formidable technical and financial challenges that stand in the way of producing a supply big enough to serve as a viable alternative to the real thing, he says.
Biologists and chemists
In his article, Neeves categorizes research efforts into creating synthetic blood under two broad headings: The biologists’ approach and the chemists’ approach.
“The biologists’ approach coaxes stem cells into becoming blood cells by growing them in bioreactors that recreate important features of the bone marrow, where blood cells are made in the body,” he writes. “The chemists’ approach synthesizes molecules and particles that mimic the functions of blood cells using methods suitable for large-scale manufacturing, thereby creating blood replacements that can be transported and stored more easily than cell-derived blood.”
Neeves says that while the biologists’ approach generally seeks to grow blood cells in flasks or tanks that perform many of the functions of natural blood, the chemists’ approach strives to engineer products than can perform specific tasks of blood, such as transporting oxygen or promoting clotting.
Cultured blood cells
Describing progress on the biologists’ approach, Neeves tells of research in France in 2011 in which extracted stem cells from a person’s blood were used to culture blood cells outside the body. But that method required drawing blood before synthetic blood could be produced.
More recent approaches involve reprogramming human cells genetically to create lines of “pluripotent stem cells” that can divide and make blood cells infinitely and can also be engineered to produce specific blood types. But the technical requirements of that method are exacting, Neeves says, estimating the cost of one unit of cultured red blood cells at $8,000 to $15,000 compared to $250 for red blood cells provided by human donors.
In a 2022 trial, researchers in Japan transfused a 55-year-old woman with cultured platelets, and a phase I trial involving cultured red blood cells is under way in the United Kingdom.
“While the trial marks a promising start to testing synthetic blood in patients, the exorbitant costs of making lab-grown blood mean that larger clinical trials – an important stepping stone toward clinical use – may still be several years away,” Neeves writes.
Wrapped in liposomes
As for the chemists’ approach, Neeves recounts early attempts at creating artificial products imitating discreet blood functions using chemicals and proteins, but those experiments led to flawed results.
More recent research involves using chemically modified hemoglobin, the protein that red blood cells use to transport oxygen through the body. The hemoglobin is encapsulated in liposomes synthesized from the molecules that make up the membrane of cells to prevent certain cardiovascular and kidney side-effects. The liposome wrapper also helps ward off the body’s immune reaction. A 2021 study showed encouraging results.
This sort of liposome technology has already been approved by regulators and is widely used for vaccine and drug delivery, Neeves says. Other chemical research is underway to create particles that mimic the functions of platelets in clot formation.
“The chemists’ approach draws upon a long history of drug delivery technologies, many of which have already gone through clinical trials and into use,” Neeves writes. “Artificial blood made in this way is therefore cheaper to make and easier to manufacture than blood made using stem cells.”
Microbots to the rescue
As a chemical engineer, Neeves sees more potential in the engineering approach to expand to mass production of usable synthetic blood products more cheaply and easily than blood made using stem cells.
“The big issue with the biologists’ approach is scaling,” he says. “It’s really the same issue that lab-grown meat has run into. You can make it at a small scale in a flask, but when you want to make, say, thousands of liters of blood, it’s hard, not just because of the technology, but the price is prohibitive. I think the economics of it will dictate what ends up happening.”
He notes that the U.S. Defense Department’s Defense Advanced Research Projects Agency is spending heavily to back research into ways to speed up transfusions to wounded soldiers lacking ready access to human blood products.
Neeves wraps up his article by peering into a future when synthetic blood cells, which circulate throughout the body, could be engineered to play roles in diagnostics and drug delivery. He also cites research into using “microbots” coated with blood cell membranes to evade the immune system’s defenses – tiny “biohybrid” devices that could be programmed to remove pathogens from the blood. Neeves himself has been researching ways to use microbots to dissolve clots for stroke patients.
“The future of synthetic blood awaits our ability to master and direct the symphony of interactions within blood,” he concludes in his article. “After all, synthetic blood is not just about replacing lost blood; it’s about revisioning what blood can do, turning a life-sustaining fluid into a dynamic and intelligent system that could address current shortcomings in transfusion medicine and improve patient outcomes in previously unimaginable ways.”