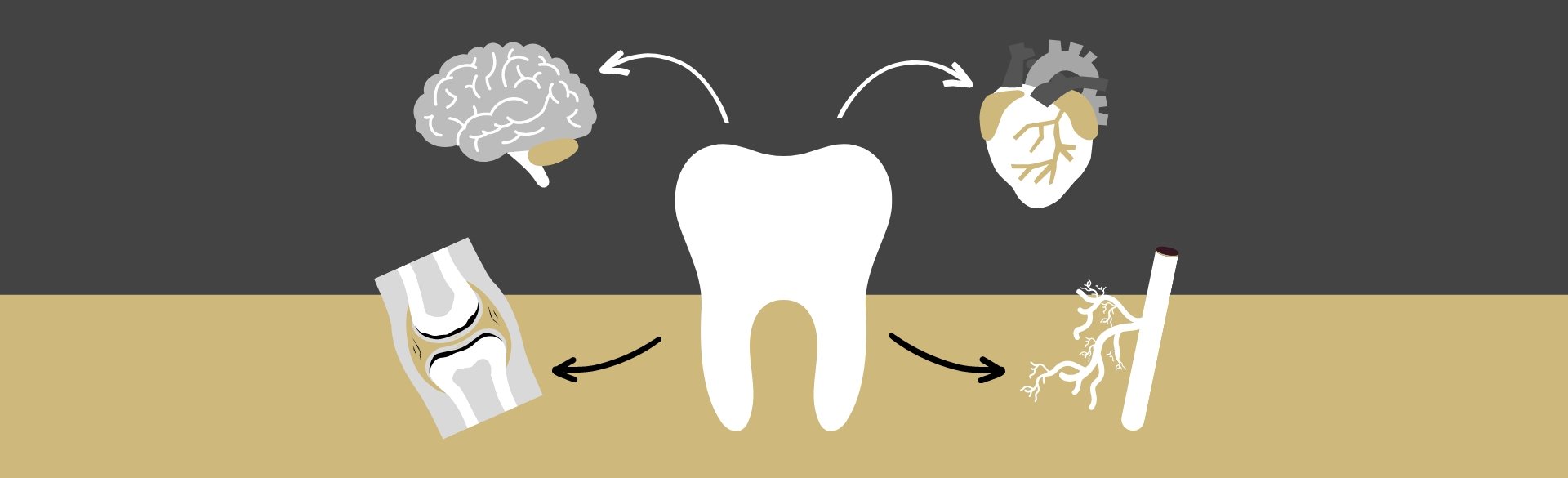
What happens in the mouth doesn’t always stay in the mouth. That’s the mantra for many dental experts today, as research into connections between gum disease and systemic disorders – from strokes and rheumatoid arthritis to diabetes and Alzheimer’s disease – becomes more prominent.
Although more studies behind the suspected links are needed, one thing is clear, said Sangeetha Chandrasekaran, MS, BDS, chair of the Division of Periodontics in the University of Colorado School of Dental Medicine: Any flossing or dental checkup resolutions made for the new year certainly can’t hurt.
“What happens in the mouth does impact other parts of your body,” Chandrasekaran said. “There’s some evidence, for instance, that patients who have periodontitis (gum disease) are twice as likely to have a stroke compared to patients who don’t have periodontitis.”
A modifiable risk factor
Strong evidence of a two-way relationship between type 2 diabetes and gum disease, an area of research focus for Chandrasekaran, also exists. “That’s a really well-established connection,” she said. “Patients who have severe periodontitis may not have full control of their diabetes, and patients who have poorly controlled diabetes may be at a higher risk for developing periodontal disease.”
Unlike a genetic predisposition, gum disease is a modifiable risk factor, Chandrasekaran said, underscoring the importance of further research and education. “This is a condition that we can treat. If it’s also a way to reduce the complications of other diseases, it’s like the ‘killing two birds with one stone’ saying.”
What is gum disease?
Gum disease begins with gingivitis, when sticky, germ-filled plaque and tartar build up, causing mild bleeding and inflammation of the gums. Gingivitis is reversible with good oral care and treatment.
The more serious periodontitis develops when infected gums begin pulling away from the teeth, creating pockets that serve as reservoirs for harmful bacteria. Periodontal care can minimize bacteria and eliminate or reduce pocket growth. Untreated, periodontitis leads to bone and tooth loss.
“Having periodontal disease really increases the inflammatory burden on the body.”
– Sangeetha Chandrasekaran, MS, BDS
While bacteria in a healthy mouth can live in peace with the rest of the body, with gum disease, escaping bacteria are more likely to cause damage, coming in more frequent and intense assaults, Chandrasekaran said.
A dangerous tag team
Bacteria associated with gum disease, such as the most common P. gingivalis, can enter other parts of the body and cause damage directly or indirectly. Some of those bacteria have been associated with systemic diseases, including Alzheimer’s and stroke.
“The other big biological factor is inflammation,” Chandrasekaran said. “Having periodontal disease really increases the inflammatory burden on the body.” The bacteria trigger the body’s immune response, and that persistent assault results in chronic inflammation, which is increasingly associated with severe disease.
As with gum disease-related bacteria, inflammatory markers have been found in high concentrations in other parts of the body in patients with periodontitis and chronic disease, Chandrasekaran said. “So it really increases the possible mechanisms.”
More research needed
Finding those mechanisms is crucial to confirming a causative role of periodontal disease in other systemic diseases. So far, only associative links have been found, largely based on epidemiological studies and animal studies, Chandrasekaran said.
Research into the connections has already led to collaborative studies across disciplines on campus, and Chandrasekaran said she hopes the research helps break down the walls between the dental and medical professions in general, leading to improved, holistic patient care.
“We have to get beyond working in silos,” Chandrasekaran said, noting that dentists often see patients more regularly than other medical providers and could make a big difference with prevention. “How do we co-manage these patients? Those questions are becoming very relevant. There has to be a broader integration, and all of this research could lead to that integration.”
Digging Deeper: Research Snapshot on Mouth-Body Connection
Diabetes
Prime suspects: Diabetes and some drugs used to treat the disease reduce production of saliva, a main defense against bacteria in the mouth. Diabetes can also increase the amount of blood sugar (glucose) in saliva, feeding bacterial growth and plaque buildup.
Campus work: CU dental researchers have teamed up with scientists at the Barbara Davis Center for Diabetes (BDC) in search of answers and biological markers, medical signs that dentists and doctors could use for treatment and prevention. Chandrasekaran is currently working with the BDC on a study looking at bacterial changes and potential biomarkers in the mouths of patients with type 1 diabetes.
Heart Disease and Stroke
Prime suspects: As pockets in highly vascular infected gums grow, the onslaught of toxic bacteria floating around the body also grows. The persistent toxins lead to inflammation of the arteries and the heart, a chief cause of cardiovascular disease.
Campus work: CU dental researcher Kerri Font, DDS, recently received an AB Nexus grant with Chris DeSouza, PhD, of CU Boulder’s Integrative Physiology department, to explore extracellular vesicles as mediators of stroke with periodontal disease. The project’s goal is to identify mechanisms and thus therapeutic targets to reduce stroke risk in patients with gum disease.
Rheumatoid Arthritis
Prime suspects: The bacterial/inflammation connection is the prime suspect in the association between gum disease and rheumatoid arthritis. In particular, P. gingivalis and Aggregatibacter actinomycetemcomitans have been identified as triggers for both diseases.
Campus work: CU dental researchers have teamed up with faculty in the Division of Rheumatology, including Kevin Deane, MD, looking at the role of periodontal inflammation in the development of rheumatoid arthritis or as a trigger for future RA.