First, explain what exactly Candida auris is and how long it’s been around.
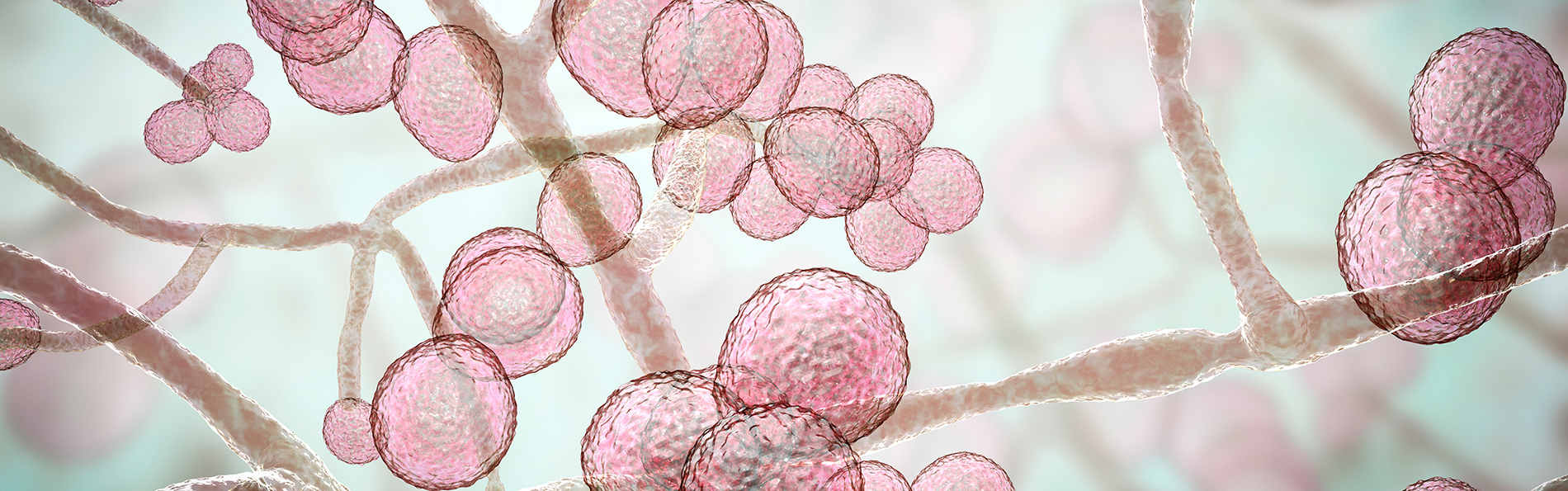
It’s a fungus that was first identified in the ear of an elderly Japanese patient in Tokyo in 2009. Since then, it’s been found throughout the world, and it probably existed long before it was first identified.
Why is Candida auris suddenly coming back up in the news – particularly in hospitals – and who is at the most risk?
We’re concerned now because it is showing up more frequently in a variety of high-risk areas like intensive care units (ICU). Much like staph infections that are resistant to antibiotics, such as methicillin-resistant Staphylococcus aureas (MRSA), some strains of Candida auris are resistant to many antifungal medications. Typically, it doesn’t infect healthy people, but it impacts the immunocompromised. Immunocompromised patients who are in the hospital can get a severe Candida auris blood infection. The infection spreads quickly and can kill one in three patients.
What are the symptoms and where does it present the most danger?
The thing we are most worried about is this bloodstream infection in people who are already critically ill. Symptoms are fever, sepsis and organ failure. Healthy people can be carrying this fungus but have no symptoms, which makes it easy to pass on to an immunocompromised person. Infection control is very important because you want to prevent it spreading from a healthy person to a sick patient, especially those who have long stays in the ICU.
What steps can healthcare providers take to help slow down the spread of Candida auris, which is resistant to antifungal treatments?
We need to develop new medications and continue strong infection control practices. Healthcare providers should be consulting with infectious disease experts on using antifungals judiciously when there are questions, so we don’t encourage medication-resistant organisms. The overuse of antifungals may be making things worse. It is vital that we use them only when needed.
It’s a very “Last of Us” plotline to say that we all have fungi living in our bodies, but we do. Talk a little bit about that and what makes it such a welcoming habitat for them.
Fungi live on our bodies. We have a symbiotic relationship with them, and they normally reside on our skin and in our gut without creating any issues. As long as they don’t invade our bodies, they don’t cause a problem. It is when our immune system is low that they can cause a problem. This is why it’s important to maintain a good weight, exercise, eat well, sleep and wash your hands to encourage a healthy immune system.
Are there any steps you can take to prevent or limit your risk of getting Candida auris?
Practice the normal healthy hygiene your doctor recommends and wash your hands regularly. As with antibiotics, antifungal medication should be used only when it is really needed.
What can friends/family do if they have an immunocompromised person in the hospital to protect them from Candida auris?
Visitors should follow infection control guidelines to lower the risk. Wear a mask, gloves and make sure you wash hands before entering the room. It’s important for healthy people to remember they may be carrying Candida auris (and other microbes) and not even know it.
Is there anything you want to add?
The issues surrounding Candida auris underscore the importance in investing in strong public health surveillance programs and infectious disease defense. Given climate change and the speed of global travel, there will be new infections that pop up, and we need to be prepared for them. The COVID-19 pandemic was a prime example of this.


.png)
.jpg)
