As the nation moves into the least-infectious period since the start of the pandemic, with Colorado’s governor last week ushering the healthy and fully vaccinated back into a mask-less and more normal life, some experts warn against moving too fast.
Concerns focus on an emerging omicron subvariant coined BA.2, which the World Health Organization recently reminded is a “variant of concern,” the durability of COVID-19 vaccines and the risks of the unknowns.
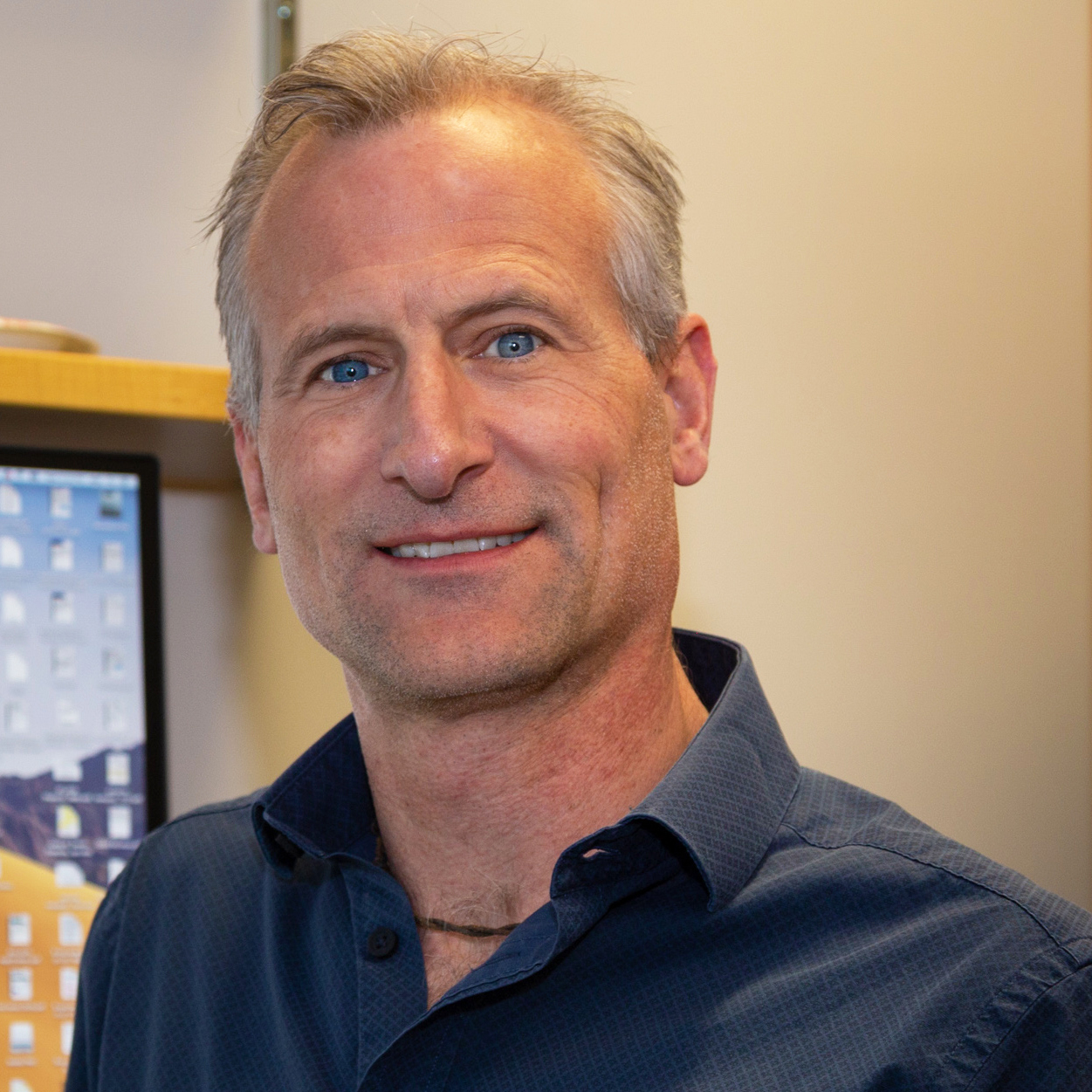
Yet other experts, including Dean Jonathan Samet, MD, MS, of the Colorado School of Public Health and Professor of Immunology and Microbiology Ross Kedl, PhD, at the University of Colorado School of Medicine, predict the time is right.
“I would say, and there are others who would agree, that this is where we are now,” Kedl said. “We’re not in the run-and-hide phase of the pandemic, but in the controlled exposure phase.”
1: BA.1 and BA.2 similarities outweigh differences
While BA.2 shows signs of nudging out its BA.1 cousin, already becoming the dominant strain in some countries, concerns of a new, BA.2-driven surge are low. Despite some experts emphasizing its estimated 30% higher transmission rate over its first-dominant cousin as cause for alarm, Samet and Kedl predict the similarities of the two omicron subvariants are more important.
“From what I know about BA.2, I don’t think we’re going to have another surge,” Samet said. “It does not have a greater degree of immune escape as far as we know. And from what information we have in hand, it looks like our vaccines and naturally acquired immunity should be as effective against BA.2 as against BA.1.”
New campus protocols
fall in line with state
recommendations.
Review the changes and the
“It’s not sufficiently different,” Kedl said. “It simply seems as though, within the omicron family of strains, it’s having some sort of an advantage in transmissibility. But It doesn’t appear to be any more dangerous to people than the original omicron variant.”
2: Case numbers dropping rapidly worldwide
In recent weeks, U.S. infection rates have continually fallen, last week registering a 65%, 14-day drop. With hospitalization and death rates steadily declining, a light is shining at the end of the COVID-19 tunnel. And it’s likely too strong for BA.2 to snuff out, Kedl and Samet said.
“All omicron infections are plummeting dramatically across the globe,” Kedl said. “That’s another reason a BA.2 takeover is certainly not exceptionally concerning to anybody who is really paying attention to that fact.”
The most recent modeling report by Samet and state university colleagues found the seven-day average of reported cases dropped from omicron’s peak of 13,800 on Jan. 10 to 1,500 on Feb. 16. The report projects a continued decline into the summer months.
“So we are definitely in Colorado heading in the right direction very quickly,” Samet said. “And I don’t think that BA.2 is going to interrupt that.”
3: Vaccine and anti-viral therapy holding up
Despite a drop in vaccine effectiveness against omicron BA. 1 infection, breakthrough cases were often mild and rarely deadly, especially in boosted people with no high-risk medical conditions. Protection against severe disease remained strong, with effectiveness ranging from 93% to 99% in some studies.
“So we are definitely in Colorado
heading in the right direction very quickly.
And I don’t think that BA.2 is going to interrupt that.”
– Dean Jonathan Samet, MD, MS
“The vaccines stand up to omicron incredibly well, and there’s no reason to believe the vaccines won’t continue to stand up,” Kedl said.
Although early evidence suggests the monoclonal therapies effective against previous COVID-19 strains are not proving effective against BA.2, the anti-viral medications appear to work against the subvariant.
4: BA.2 faces dramatically higher world immunity
Many experts, although not all, view the highly transmissible but less deadly omicron as the catalyst for ending the dragging pandemic.
“The fact that omicron spread so broadly has increased overall levels of immunity within the broader public,” Kedl said. For vaccinated and boosted people with no comorbidities, the risk of severe omicron is “lower than the risk you take getting into your car every morning,” he said.
Modeling report experts estimate that 90% of Coloradans have some immunity, natural and vaccine-induced, against SARS-CoV-2.
“There was a time and a phase in the pandemic in which we needed to isolate and separate in order to reduce transmission,” Kedl said.
“We are unmasking now not because there is no chance of getting infected, but because the vaccines have made it safe to do so.” What that means is that for those with some immunity and low risk of hospitalization, exposure to the virus and maintenance of immunity within the community is a safer and necessary path forward, Kedl said. “What’s going to protect the vulnerable the best is if the rest of us have as high immunity as possible.”
5. Subvariant can help keep immunity up
Garnering the highest level of immunity means accepting the risk of infection for those not at high-risk of hospitalization and maintaining booster schedules as they roll out.
Fourth shots are already recommended for the immunocompromised. For the general public, Kedl estimated a need for second boosters “in the eight-months-to-year-and-a-half range.”
“A lot of it depends on what the next variant happens to be. If omicron stays circulating, it’ll eventually hunt you down, because your immunity will wane enough, but all the data indicate you should more than have enough immunity to get through it safely while it kicks your immunity back up,” Kedl said.
“What’s going to protect the vulnerable
the best is if the rest of us have as high
immunity as possible.” – Ross Kedl, PhD
“If a new variant that is really different spins out in three months, that could be a different story. I find that unlikely, but that would be the circumstance that would most likely compromise the durability of this last booster.”
6. Vigilance must remain for at-risk and health experts
Older Americans and people with other high-risk factors should still mask up in public, Samet said. With the evolving transmissibility of SARS-CoV-2, N95 and KN95’s should be a first choice, as they help filter out more of the smaller aerosols than cloth masks, he said.
As for the change in public health policies, Samet predicts they are pointed in the right direction. “I think when things are down and infection is not particularly prevalent in the population, it’s the time to say, ‘OK, now it’s the time to relax our infection control measures,’” he said.
“Projections show we should be heading back to prior lows of infection in the state. The big unknown is how long our immunity will last, whether it’s from vaccination or naturally acquired, and what nature might bring us in the form of the next variant.”
While a surprise, more severe variant could change the path again, Kedl, based on virus behavior, finds it unlikely. “Some experts are stressing the fact that there is no guarantee the next variant won’t be worse than omicron. That’s always possible, but in my opinion, it is by no means the most likely,” he said.
Like BA.2, the way a virus survives generally is to become more transmissible but less virulent, Kedl said. “Whatever comes next will have to beat out omicron, and that’s not going to be an easy thing to do.”