A research team with a faculty member from the Colorado School of Public Health at the CU Anschutz Medical Campus has found that stroke risk has dropped in both black and white older adults. The study analyzed 25 years of Medicare hospitalizations due to stroke.
The study publishes today in the April issue of Medical Care.
The findings are important because black Americans have shown consistently to be at a higher risk of strokes. This study reveals hospitalization rates have decreased in both races; however, black patients had a greater reduction in mortality. Though, black men and women continue to be at higher risk for stroke than white patients.
“Our findings show encouraging declines in stroke hospitalizations and mortality in older adults most likely due to smoking reductions and the increasing use of medications that control risk factors. However, the study also sheds light on critical unresolved disparities in the risk of stroke among minorities,” said Marcelo Perraillon, PhD, assistant professor at the Colorado School of Public Health.
Marcelo Perraillon, PhD, assistant professor at the Colorado School of Public Health
Colorado Stroke Trends
In Colorado, strokes are the fifth leading cause of death, a relatively lower stroke incidence than the average in the US. However, race and income disparities are a concern for incidence and mortality rates on both a local and national level. Similar to national trends, poorer counties in Colorado, as well as black and Hispanic residents, have higher stroke risks and mortality rates.
New Study Finds a Decline Over 25 Years
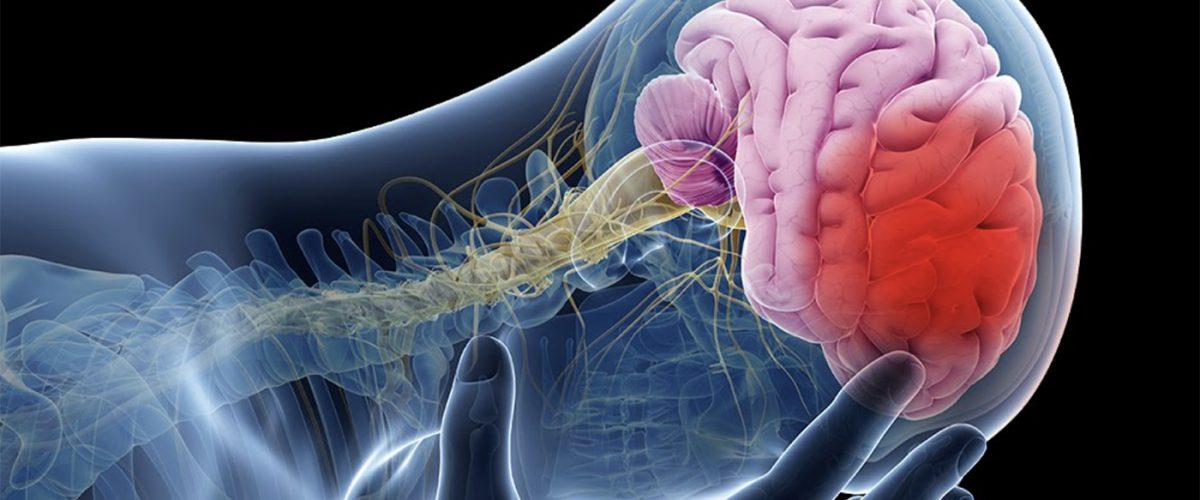
Using Medicare data from 1988 to 2013, the researchers on this study analyzed trends in hospitalization and mortality after an initial stroke in black or white men and women aged 65 or older. The study included more than 1 million hospitalizations for ischemic stroke, caused by blockage or narrowing of the brain blood vessels; and nearly 150,000 hospitalizations for hemorrhagic stroke, caused by bleeding into or around the brain.
Over the 25-year study period, hospitalizations for stroke decreased for both black and white patients. Adjusted for age, ischemic stroke risk decreased from 1,185 to 551 per 100,000 Medicare beneficiaries among black men and from 932 to 407 per 100,000 among white men. Risk fell from 1,222 to 641 per 100,000 for black women and from 892 to 466 per 100,000 for white women.
Mortality after ischemic stroke also fell, with greater reductions in black patients. Risk of death within 30 days after ischemic stroke decreased from approximately 16 to 8 percent in black men and from 16 to 12 percent in white men. Ischemic stroke mortality declined from about 14 to 9 percent in black women versus 16 to 15 percent in white women.
Although the study can't show a causal relationship, the reductions in stroke hospitalization and mortality were accompanied by declines in key risk factors: particularly smoking, blood pressure, and cholesterol levels. The improvements in stroke outcomes occurred despite the worsening US epidemic of diabetes and obesity.