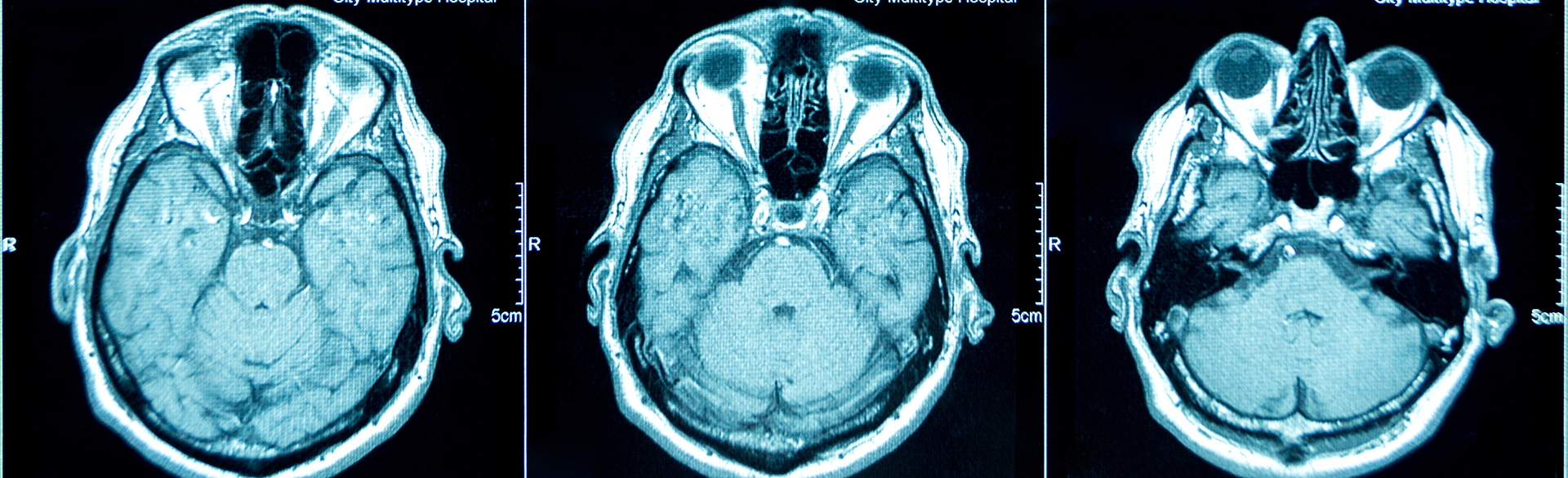
Researchers from the University of Colorado School of Medicine have released a study that shows that a new imaging method “fast MRI” is effective in identifying traumatic brain injuries in children, and can avoid exposure to ionizing radiation and anesthesia.
The results of the study, which are published in the journal Pediatrics, establish a new, low-risk way to test for brain injuries. The study was designed to determine the feasibility and accuracy of “fast MRI,” or magnetic resonance imaging, when compared to computed tomography (CT) scanning.
“We found that fast MRI is a reasonable alternative to CT,” said Daniel Lindberg, MD, associate professor of emergency medicine at the CU School of Medicine and lead author of the article. “Nearly all – 99 percent – of fast MRIs were completed successfully, with accuracy that was similar to CT, while avoiding the harms of radiation exposure.”
Each year as many as 1.6 million children visit U.S. emergency departments with a concern for traumatic brain injury. As many as 70 percent undergo CT scanning, which exposes the children to ionizing radiation and increased risk of cancer.
Conventional MRI can identify injuries without radiation exposure, but requires the child to remain motionless for several minutes. Conventional MRI requires anesthesia, which is not practical in many injured children and may expose them to mild cognitive injury. Fast MRI avoids the need for sedation by using faster, and more motion-tolerant imaging techniques.
Between June 2015 and June 2018, the CU researchers recruited participants to their study. Children less than six years old who had already undergone CT scans during their emergency care were eligible to participate and those enrolled received fast MRI as soon as possible, usually within 24 hours of the CT scan.
Of the 225 children enrolled, fast MRI was completed in 223. The median imaging time in fast MRI was 6 minutes, 5 seconds. Fast MRI results matched those of CT in greater than 90 percent of cases. CT showed better accuracy for identifying fractures or breaks to the skull, while fast MRI did a better job of imaging the brain and the space between the brain and skull.
One limitation of the study is that it may not apply to other settings without access to cutting-edge MRI scanners or experienced pediatric radiologists. “We were fortunate to be using newer scanning equipment and highly experienced technicians and pediatric radiologists,” Lindberg said. “While we believe our findings reveal a feasible alternative to CTs in pediatric specialty centers, further study is necessary to test the results in other settings.”
In addition to Lindberg, nine other CU School of Medicine faculty members are co-authors of the study: Nicholas V. Stence, MD, Joseph A. Grubenhoff, MD, MSCS, Terri Lewis, PhD, David M. Mirsky, MD, Angie L. Miller, MD, Brent R. O’Neill, MD, Kathleen Grice, Peter Mourani, MD, and Desmond K. Runyan, MD, DrPH.
Guest contributor: CU School of Medicine
.png)
.jpg)
