When 17-month-old Wrenn died in her sleep unexpectantly it was devastating to her family, including her aunt – University of Colorado College of Nursing Assistant Professor Emily Cheshire, DNP, MS, FNP-BS.
“When this happened, it was obviously a tragedy, and I had no answers,” Cheshire says. “There was nothing in my 17 years of experience (as a nurse and medical provider) and nothing in my education to prepare for this. I had never heard of Sudden Unexplained Death in Childhood or SUDC, and I realized there was a knowledge gap.”
SUDC is not the same as SIDS (Sudden Infant Death Syndrome), which has received considerable publicity and funding in recent years and thus has identifiable risk factors. SUDC is the sudden death of a child older than one year of age (up until the age of 18) that is unexplained after a thorough investigation. The CDC reported 450 cases of SUDC in 2021, with 55% of those deaths happening to children ages 1-4, but the number of cases is likely higher.
“Any pediatric death defies the natural order that defines the human experience,” Cheshire says. “It can be shocking, and it can affect people in different ways. Talking to people who have been through it and know what that level of loss feels like can be really powerful and less isolating.”
What Happened to Wrenn?
Wrenn was found unresponsive one morning at her home in North Carolina. Cheshire says the day before, Wrenn had a slight temperature, a raspy voice, and a small cough. She was otherwise perfectly healthy without any medical conditions, was current on vaccines and had normal growth and development.

Emily Cheshire, DNP, MS, FNP-BS, with her niece Wrenn when she was six months old |
“When we think about that clinically, it’s not a big deal for a 17-month-old to have those symptoms,” she says. “On the autopsy, her official cause of death was complications of viral upper and lower respiratory tract infection, including COVID-19 and the flu. But when we correlate that with her clinical presentation the day before, it doesn’t add up. The question truly becomes: Did she die of COVID-19 or the flu, or with COVID-19 and flu?”
Cheshire also says there is video footage of Wrenn having a seizure overnight before her death that would not have been known without the video. Seizures and arrythmias rarely leave evidence at autopsy to confirm or deny their occurrence. “Wrenn had no prior history of febrile seizures, and we do not know if that contributed to her death,” Cheshire states.
“We also don’t actually know how rare SUDC is, and one reason is because of the variability of investigation and death certification practices across states, and counties,” Cheshire says. “Sometimes, when mild pathology alone is found on the autopsy, it may be ruled as an explained cause of death, potentially underestimating SUDC. Research published in JAMA Open Network by the SUDCRRC at NYU Langone Health in 2020 found that blinded reviews of sudden deaths in children showed >40% discordance with the original death certification.”
Cheshire explained more research and thus funding is needed. SUDC has no identifiable risk factors and is therefore unpreventable at this time.
Wrenn’s cause of death is undergoing a multi-specialty review, which means healthcare professionals will either agree with her cause of death certification, consider a different cause of death, or consider her death unexplained with the information currently available.
“In Wrenn’s case, we have video of that seizure,” Cheshire says. “If this happened to my own children, I wouldn’t have had video evidence, so I wonder if more cases with video evidence could teach us more."
Helping Parents & Families Cope
Cheshire’s sister and brother-in-law found support and resources through the Sudden Unexplained Death in Childhood Foundation. The SUDC Foundation raises awareness, funds research, and supports those affected by SUDC. The SUDC Foundation provides all services at no cost to the people it serves.
“My sister has been paired with other people who have been experiencing the grief and trauma that accompanies the loss of a child, which has been really helpful to her since it’s hard to relate,” Cheshire says. “The SUDC Foundation also acts as the liaison between families and a coroner or medical examiner’s office to assist in understanding autopsy results, because those are really confusing and complex systems.”
In 2016, The SUDC Foundation awarded a scientific grant to the National Association of Medical Examiners to convene a consensus panel to evaluate the literature and formulate national guidance in this area. The final publication "Unexplained Death In Pediatrics: Investigation, Certification and Family Needs" is publicly available through the National Library of Medicine. In collaboration with the American Academy of Pediatrics, an expert panel convened to create the first national procedural guidance relating to pediatric deaths. The guidelines include standardizations for autopsy, certification practices to improve accurate surveillance, trauma-informed protocols, training first responder teams, educating hospitals, and collaboration between medical professionals and other agencies.
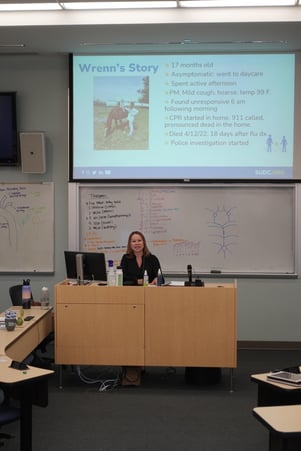
Cheshire presenting Wrenn's story and information about SUDC during CU Nursing's Grand Rounds in October |
“It’s important to make sure when families leave the hospital, or if they’re at home, that they have materials that explain the medical and legal systems,” Cheshire says. “It’s important for the hospital to have a point person, like a social worker, that the family can call. If the death occurs at home, the primary care provider for the child can play a critical role in helping the family navigate the systems and ensure referrals for mental health and grief support are in place. The family is in shock, they don’t know what to ask. They need a person to check in on them.”
Families should expect a death investigation to happen immediately and prepare for police and child protective services to ask them questions.
“The investigation is routine, but parents and families need anticipatory guidance,” she says. “One family said they left the hospital with a piece of paper on grief, and then were contacted by child protective services and a medical examiner and thought they were in trouble.”
The SUDC guidelines also suggest giving families a private room at the hospital to grieve, allowing families to hold the child, and providing families with memorial keepsakes such as a handprint or footprint. Other resources include bereavement information for support groups for families, siblings, and other relatives.
The Role of Medical Providers
“Hopefully this never happens to anyone, but if it does, it’s really important to get everything right,” Cheshire says. “Those families remember those healthcare and medical providers. So what we do and don’t do for families during this time matters.”
Cheshire says since her niece’s death happened at home – not a hospital – the death investigation started at her sister and brother-in-law’s home, so there was no primary healthcare provider around, except for EMS.
“Our role as the child’s primary health care provider becomes more important because there is no hospital contact,” Cheshire says. “We can serve as a liaison between the medical examiner and pathologist and help the family with bereavement resources.”
Cheshire says she’s seen SUDC cases where a medical provider’s malpractice lawyers told the provider to cease contact with the family. She says this can cause prolonged grief and trauma for families.
“I think there’s a way we can say ‘I know you want answers, and it’s normal to look for a cause of death, and if there’s something I missed, I’m going to find answers’, “’ she says. "We as medical providers can come out of that uncomfortable place and still support the family.”
Raising Awareness of SUDC
Wrenn's case was registered with the SUDC Registry & Research Collaborative (SUDCRRC) funded in part by The SUDC Foundation. The SUDCRRC is the largest multi-site research collaborative on SUDC and was created at NYU Langone Health in 2014 by Orrin Devinsky, MD, and Laura Gould, MSc. The SUDCRRC studies sudden unexplained deaths in childhood (SUDC) with their team of experts from pediatrics, neurology, cardiology, radiology, pathology, and infectious disease to better understand and learn to prevent these tragedies. By combining the knowledge of academic investigators, forensic pathologists, medical examiners, and coroners, they have explained deaths that have been previously unexplained. Families who participate can receive study results as they help to advance medical research, which may assist with anxiety as a result of the sudden inexplicable death. “As you can imagine, the choice to have another child after the unexpected death of one child can be extremely difficult for parents,” says Cheshire whose sister had another child since Wrenn’s death.
|
What is the Difference Between SIDS, SUDC, and SUID?
|
Cheshire is now an ambassador with the SUDC Foundation. She says she will be following along with new research and is open to presenting information about SUDC to bring more awareness about this category of death.
“Through the support of the SUDC foundation, we found out Wrenn’s case wasn’t necessarily unique,” she says. “My hope is – and why I think it’s important to bring awareness to this category of death – we as medical providers can be a source of support and advocacy in the aftermath for these families. It matters.”
March is SUDC Awareness Month, and people can show support by wearing blue and yellow. The SUDC Foundation’s website has information about SUDC, resources, and support for families, and ways to get involved with the foundation.



