When University of Colorado College of Nursing student Rebecca Feldman was delivering hydromorphone through an intravenous drip to an injured patient, the new medical device she was using started flashing “Occluded! Occluded!” For a moment, she didn’t know what to do. Fortunately, it was just a test. Feldman was taking part in an exercise with other nursing and bioengineering students at the University of Colorado to test medical devices and improve healthcare.
“The idea here is to have the future creators of these medical devices and the future users of these devices be able to really embrace this collaborative relationship to provide better outcomes for patients in the future,” says Morris Huang, PhD, assistant research professor in the Department of Bioengineering at the University of Colorado Denver and the Center for Inclusive Design and Engineering (CIDE).
Putting the End-User First
Dr. Huang created the exercise two years ago for students in the Department of Bioengineering and the College of Nursing. He wanted to teach his students to think about the end-user at all stages of a design.
“While they probably have the best interests of their users at heart, it is important to still take whatever you've created, hand it to the user, and allow them to work with it so that you can understand if, and where, things need to be improved,” says Huang.
Small Groups Help Identify Majority of Issues
|
|
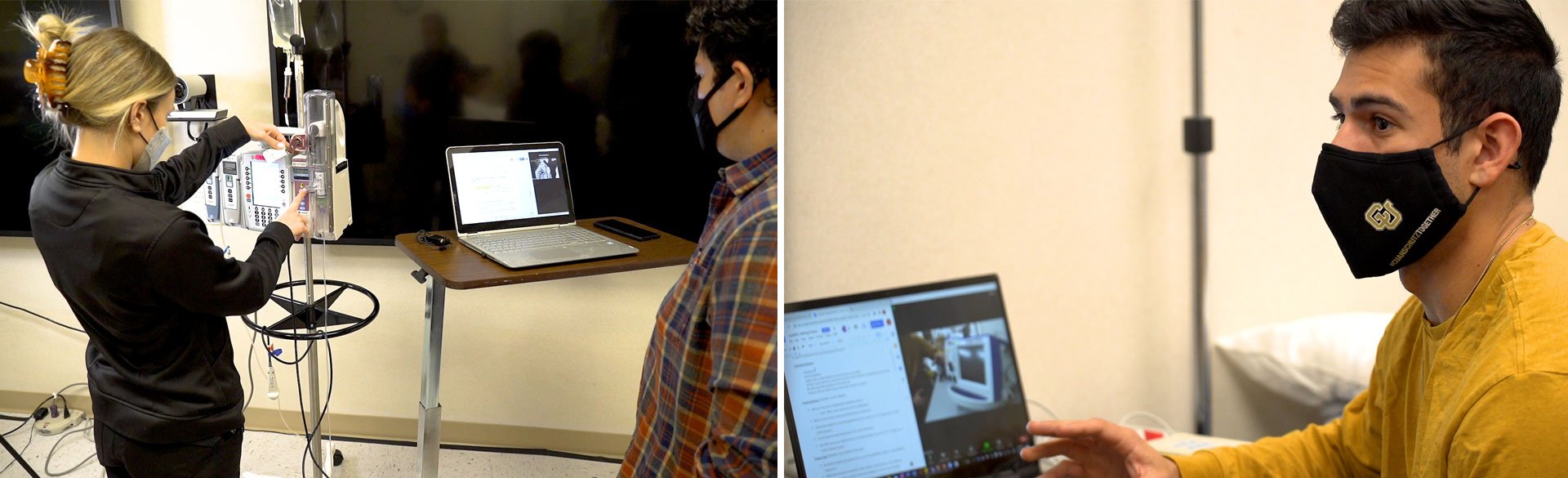
Students were separated into small groups of six students per team. “Literature suggests that even five testers can be invaluable – identifying 85% of user issues,” says Huang. During the exercises, the engineering students set up cameras and laptops in the simulation center at UCHealth to record nursing students as they try to use medical devices in real-world situations like heart attacks. When they’re finished, the engineering students ask them how hard the devices were to operate, when and where instructions were confusing, and what clarifications and improvements were needed.
“It was really awesome for them to get our input while we test their equipment,” says Feldman. “We get to share what is going to work for our patients and what's going to be easier for us to use as nurses. We work with multiple patients and a lot of times we feel rushed. So, we want the machinery to work as efficiently as possible.”
Language Plays a Role in Successful Deployment
During the tests, the engineering students quickly realized their professional jargon is different from nursing lingo and caused confusion about how to use some of the devices and troubleshoot problems.
“One example from the exercise today was the word ‘output.’ As an engineer, I know that's an electrical current. But a nurse sees that and has no idea what ‘output’ or ‘milliampere’ means. So, I think it's important to see how the language we use works together and how we can bridge that gap,” says Erik Carrera, bioengineering student.
Carrera says the exercise has helped prepare him for his new job as a biomedical engineer where he will teach surgeons how to use devices during cranial facial surgeries.
“Engineers have a very specific mindset of design and how something works. So being able to see other mindsets in other career fields use the device in their setting is important,” says Carrera.
Learning to Speak the Language of Other Professionals
The usability tests will help the bioengineering students learn to speak the language of nurses and other medical professionals who will work with their devices down the road.
“I think a lot of companies prefer that an engineer has some communication, marketing, and sales chops to go along with their technical understanding and foundation. Also, they don’t just design and build the devices, but they also educate, troubleshoot, and can communicate and learn from clinicians,” says Huang.
The interface project also allows the nursing students to work with equipment they’ll soon be using as professionals. According to CU Nursing Associate Professor and Senior Director Experiential Learning Fara Bowler, DNP, APRN, CHSE, “this collaboration helps the nursing students feel comfortable voicing their opinions about technology. They discover what can work and critically think through the device. That’s really essential when they’re on the job dealing with unfamiliar surroundings and equipment, new processes, and demanding situations.”
Using Devices Seen as an Advantage for Soon-to-Be Nurses
“Being able to put ourselves in a situation where we are forced to think critically and actually use the equipment and think about how we would use it in a real-life scenario is an invaluable experience,” says Josh Maner, CU Nursing student.
“It's not often the engineering and the healthcare world intertwine. Seeing it firsthand and how they value our feedback and how we make the equipment a little easier to use could save seconds, which could save someone's life,” Maner adds.
“This provides an opportunity to contribute to healthcare before our students go into the field,” says Bowler. “It is encouraging and inspirational to have health science students creatively learn together. The synergy of respect and shared knowledge is positive for healthcare systems and patient care. This event is the intersection of CU Nursing, CU Bioengineering, and UCHealth Simulation Center.”
The idea to bring the two student groups together was Huang’s. Once the two groups came together, a true collaboration across disciplines developed – providing an appropriate learning event for both student groups that will ultimately benefit patients who need the latest technology to diagnose and treat their health conditions. Huang thanks CU Nursing, the UCHealth Simulation Center, and the Center for Inclusive Design and Engineering (CIDE) for taking a chance on his project.
“I'm very grateful to them because when I was putting this project together, it was just an idea. I reached out to different simulation centers and to different colleges and groups to try to get participants from them. The UCHealth Simulation Center and University of Colorado College of Nursing were the only ones that responded. So here we are today running it for the second year,” says Huang.
Thank you to the following for helping make this story possible:
University of Colorado College of Nursing (Senior Director Experiential Learning Fara Bowler, DNP and Kathy Foss, RN), University of Colorado Department of Bioengineering and the Center for Inclusive Design and Engineering (Assistant Research Professor Morris Huang, PhD), UCHealth Simulation Center (Alexandra Kerekes, RN, and Trevor Gardner)