CU Nursing’s July Grand Rounds presentation was a joint effort between Drs. Figaro Loresto and Scott Harpin and highlighted different ways the two harnessed their backgrounds and skills to make a difference during the COVID-19 pandemic. In March, Loresto and Harpin asked themselves what they could do to help in the pandemic – one from a research perspective and the other from a “bedside” and public health perspective. Their unique skill sets have helped and continue to help fight the epidemic in myriad ways.
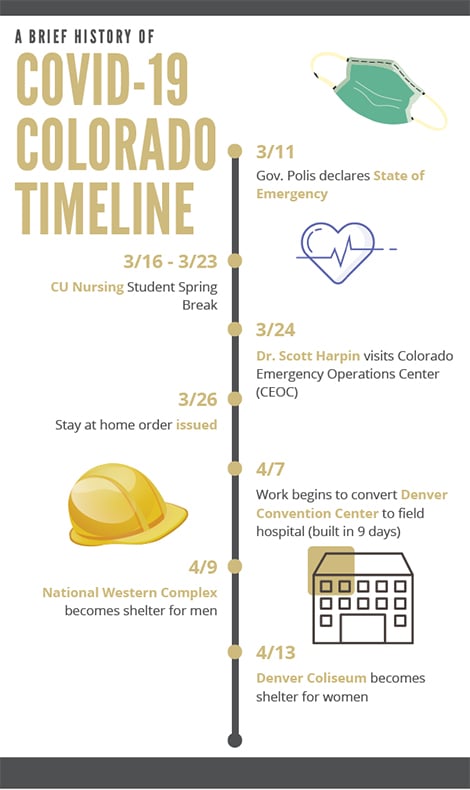
A brief history of COVID-19 Colorado Timeline
Dr. Loresto, a biostatistician and nurse scientist at Children’s Hospital Colorado used his data mining background to develop a searchable repository of the latest articles related to COVID and other epidemics including SARS, Ebola, and H1N1.“It started with 49 articles, it has grown to 761 -- with more than 500 related to COVID,” said Loresto.
His database allows practitioners to conduct robust literature searches differently than before. “Our priority as nurses is to be by the bedside. Having access to this type of information quickly helps clinicians hone in on treatment therapies and procedures that have worked in the past and might have applications for our current pandemic.”
Loresto’s vision for the repository and application is “to provide tools at your fingertips for clinicians.” Check out his application on Children’s Hospital’s website at: childrenscolorado.shinyapps.io/RN_COVID_Lit/
Harpin took a different approach to the pandemic by joining the front-lines of the state’s emergency response efforts. Having volunteered in Louisiana during Hurricane Katrina, he decided, “I could leverage those lessons learned to assist with staffing and training needs of the state emergency workforce.”
On March 24, 13 days after Governor Polis declared a state of emergency, Harpin attended his first meeting at the Colorado Emergency Operations Center. “At that time, the experts believed that Colorado would need about 5,000 ventilators and 15-20,000 non-hospital beds to handle the influx of patients if we couldn’t reduce an impending surge,” said Harpin. “We only had approximately 900 ventilators at the time, a far cry from the anticipated need.” Harpin quickly saw the magnitude of the crisis.
The team assessed Colorado and its capacity, categorizing potential cases across tiers of need from acute to non- acute requiring isolation, but not extraordinary care. “With the anticipated need for many beds for acute patients in hospitals, it became apparent that converting large facilities to make-shift hospitals was a necessity.” The questions became -- where will the patients go, who will staff for our needs, what equipment do we need to meet the demand, and what kind of training do we need?
As Colorado’s “field hospitals” were built out within days (i.e. the Denver Convention Center and The Ranch in Loveland), Harpin was developing ‘Just in Time Training’ videos and modules for health care providers and the general public. “We trained 15 master trainers, two of whom are CU Nursing alums!” said Harpin. Those trainers are prepared to train hundreds of first-line responders including health sciences students, retired RNs/MDs, Medical Reserve Corps members, health care workers from other hot zones and community volunteers. It is often said that successful crisis management is planning for the worst and never having to enact the plan because the crisis has been averted or abated. “We hope we don’t have to use the field hospitals, but we have them ready just in case,” said Harpin.
In addition to staffing up for the public, it became clear in late March that Denver’s homeless populations were a special concern for COVID transmission. “Stay at home orders do not work for those with no home,” said Harpin. So it became imperative to create shelters with social distancing capabilities for this vulnerable population. The City of Denver organized around two facilities – a 750-bed operation at the National Western Complex specifically for men and a second 250-bed facility for women at the Denver Coliseum. “We discovered that we needed to make sure that we provide not just masks, socially distanced beds, but also an array of social services to include medical and behavioral care,” said Harpin.
“These facilities have also provided much-needed clinical opportunities for our students,” said Harpin. “As well as a great learning opportunity, our current experience might pepper our future curriculum with COVID-19 education.”
At the time of the presentation, the state had 1162 ventilators at the ready, and 316 were in use. As of July 17, the number of coronavirus cases and hospitalizations is slowly rising throughout the state. Moreover, the Governor has issued a state-wide mask order in response to the increase.