Pediatric ophthalmologists now have a tool to help ensure babies with retinopathy of prematurity (ROP) are receiving necessary follow-up care as the eye condition evolves in the weeks and months after birth.
Pediatric optometrist Melissa Engle, OD, FAAO, and a team of clinical application analysts launched a tracker last year that’s integrated into Epic, a widely-used electronic health records system, that automates when and how often a health care provider should follow up with a baby with ROP. Engle, who serves as the director of clinical informatics for pediatric ophthalmology in the University of Colorado Department of Ophthalmology and Children’s Hospital Colorado, worked in collaboration with Jennifer Jung, MD, associate professor of ophthalmology and director of ROP services, on the project.
Now, pediatric ophthalmologists all over the country are looking to the CU Department of Ophthalmology and Children’s Hospital Colorado so they can implement the tracking tool for their own use.
“We wanted this system to be flawless so that no baby falls through the cracks of scheduling,” Engle says.
With over a year of development, the tracker has a 100% success rate, which Engle says is a far better system than the physical ledgers or spreadsheets many providers have been using.
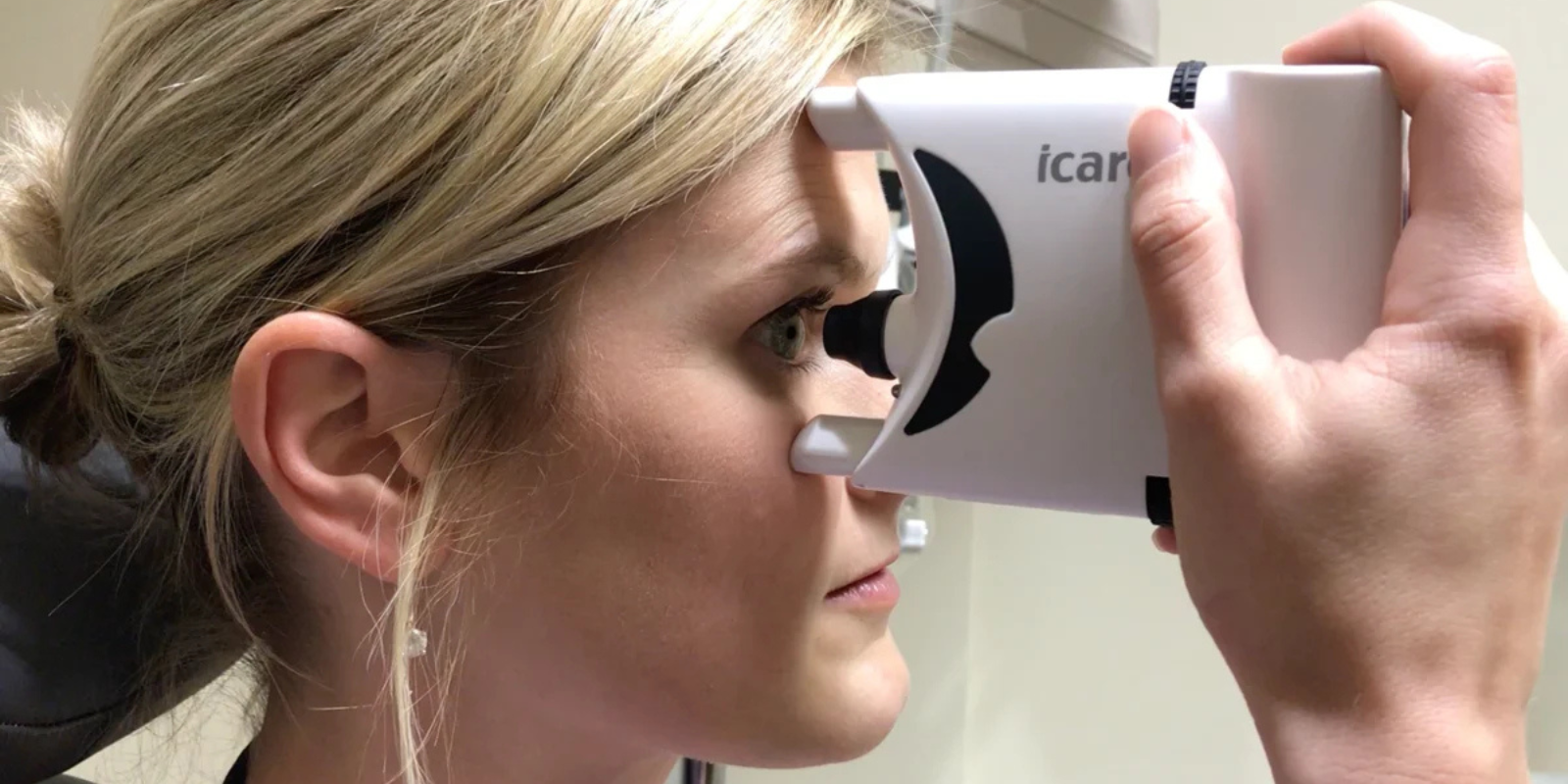
Proactive screenings
About 14,000 babies across the U.S. are diagnosed with ROP each year. The majority of cases — about 90% — are mild, but estimates show that between 400 and 600 babies become legally blind from the disease.
“When a baby is born prematurely, their blood vessels haven’t fully developed,” Engle explains. “It’s common that as vessels develop, they are abnormal and can extend into the retina, which can lead to retinal detachment and blindness.”
More severe cases of ROP require treatment, such as laser surgery or injections that help stop irregular blood vessel growth.
“We’re always monitoring babies closely to watch the severity of the ROP,” Engle says. “That’s why it’s so important to have an accurate tracking system because each baby will have a different schedule for follow up based on the severity of their exam.”
Babies at risk for ROP are born at 30 weeks or earlier or weigh about 3 pounds or less. When the tracker recognizes a baby has one or both of those criteria, the program forces a pop-up, prompting the neonatal intensive care unit (NICU) provider to schedule a ROP screening, more formally called a “ROP consult order.”
“This consult order data automatically calculates when the baby is due for their ROP screening and places them on a specific weekly report. When our ophthalmologists examine the babies, they document in a customized ROP flowsheet within Epic’s Kaleidoscope ophthalmology module to record essential follow-up data each week,” Engle says. “This data then pulls into specific ROP weekly reports to ensure each baby is scheduled for the correct follow-up week.”
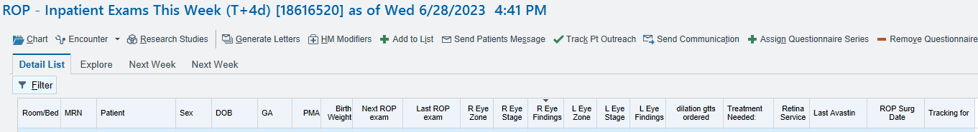
The ROP tracker Melissa Engle, OD, FAAO, developed with colleges ensures that proper follow-up scheduling occurs.
The calculations also help eye technicians work more efficiently and reduce human error.
“If you ask pediatric ophthalmologists, they say that there hasn’t been a great way to keep track of these babies,” Engle says. “It’s so important to follow up with them because they can go blind without timely treatment.”
Tracking changes
Babies that are born prematurely may be in and out of the hospital, which adds a layer of difficulty for pediatric ophthalmologists closely monitoring their patients. The tracker has built-in mechanisms that remind staff about needed follow-up examinations.
The tracker also accounts for transfer patients, offering broader insight into their medical history.
“If a baby is born at a different hospital and is seen by an ophthalmologist and then transfers, historically there wasn’t an easy way to know when their last exam was,” Engle says. “Now, we can know when they had their last exam and what the previous doctor’s guidance for follow-up care is.”
Prioritizing solutions
Providers who have used the tracker say they’ve seen a significant improvement and have remarked that the system is much more reliable than former methods of tracking.
"This new method has saved me hours of stress and made ROP workflow much more efficient,” one ophthalmologist said in a review of the tracker.
A version of the tracker will soon be built into Epic’s foundation, which is available to all of the application’s users. Epic reports that more than 305 million patients have an electronic health record in the system.
Melissa Engle, OD, FAAO, gives a presentation about the ROP tracker.
For Engle, who began her current role with clinical informatics in 2019, having the time and training to make the ROP tracker possible has been significant in building the tracker and creating a solution that has broad application.
“I have the time and resources allocated into my schedule to work on projects like this one,” Engle says. “We always knew we wanted a better way to track these babies through their care, so it was fortunate that we were able to make it happen.”

.png)