The Elliman Conference room in the Strauss Health Sciences building was filled close to capacity. Students and faculty from across the CU Anschutz Campus, healthcare professionals, along with students from Regis University, came together for one purpose: to learn how to administer naloxone to reverse a potentially fatal opioid overdose. They walked away with that, and much more.

Pharmacy students Ellie DeGagne and Nikki Kochmann welcome the audience to the naloxone event. |
The Naloxone Awareness Dinner was organized by pharmacy students Ellie DeGagne of CU Pharmacy and Nikki Kochmann of Regis University, both recipients of the annual JP Opioid Interaction Awareness Alliance Scholarship.
“As an advocate of The Alliance’s mission, I wanted to organize an event that would bring awareness to the devastating impact of the opioid epidemic, train individuals on proper naloxone use, and provide free naloxone to members of our community,” said DeGagne. “We had students from the CU and Regis Schools of Pharmacy, Medicine, Public Health, and Dental Medicine. Our work as health care providers is interdisciplinary and we each have an important role in protecting and promoting patient safety.”
Those in attendance quickly learned that the JP in the alliance’s name was far more than a generic acronym.
What’s in a Name?
JP stands for James Patrick Carroll, the son of Don and Karen Hill, the first speakers of the evening. Karen, first to take the podium, introduced the audience to JP with the enthusiasm that comes with maternal pride. She described JP as an avid athlete, a diehard Oakland Raiders fan, and a CU neuroscience grad. Sometime after graduation, JP was prescribed benzodiazepine for a mental health condition. Not long after that, JP and other members of his family were cleaning out his grandmother’s home, where he came across a bottle of unused opioid medication in her medicine cabinet.

Karen Hill introduces the audience to her son James Patrick Carroll. |
One benzodiazepine and one opioid. That’s all is took. The lethal combination of these two medications was enough to end the life of James Patrick at age 26 and forever change the lives of those he left behind.
As the audience sat in compassionate silence, Don Hill, JP’s father took the stage. Don shared memories of JP as images of family vacations and holidays flashed on the screen. He acknowledged the unspeakable pain that such a tragic loss brought to his family. But unwilling to let the story end there, Don, along with his wife, Karen, poured their pain and energy into founding the JP Opioid Interaction Awareness Alliance and partnered with the Colorado Consortium for Prescription Drug Abuse to heighten awareness about the dangers of combining opioids with other medications.
Doctor’s Orders
Suzi Stolte was next to speak. As the volunteer Director of Communications and Marketing for The Alliance, Stolte began her presentation with a brief history of the opioid epidemic. She talked about how oxycontin became the number one prescribed medication in the nation in the 1990s and how overdose deaths topped 100,000 for the first time ever in 2021.
Then, the statistics became personal. She introduced the audience to Heidi.

Suzi Stolte explains how a mixture of opioid and benzodiazepine took the life of her daughter Heidi. |
Heidi was a 37-year-old caseworker who spent her life serving others by helping them find housing and medical care. She had been taking prescribed opioids for years to counteract the pain inflicted by a car accident. Over the years her chronic pain led to depression for which her doctor prescribed a benzodiazepine. On the Friday before her death, she returned to her primary care doctor because of ongoing neck and back pain and left with another prescription for Oxycodone. On Saturday she took that medication along with her prescribed Xanax, went into respiratory distress and died. Her prescriptions were prescribed by physicians and dispensed at licensed pharmacies. However, nowhere along the way did anyone explain the dangerous interactions that can occur when mixing opioids with other medications.
Heidi was Suzi Stolte’s daughter. And, like Don and Karen Hill, she was shocked and outraged that the combination of two highly prescribed drugs could be so lethal. Several weeks after Heidi’s death in 2016, the FDA would come out with a “black box warning” indicating the dangers of taking opioids and benzos together. For Heidi, that was two months too late. Today, Stolte makes it her mission to help end the opioid epidemic by telling her story and educating others on the dangers of medication interactions.
By the time Rob Valuck, PharmD, pharmacy professor and Executive Director of the Consortium for Prescription Medication Drug Abuse, began the training portion of the event, the attendees were all ears.
Dr. Valuck focused on the history, popularity, and devastating effects of fentanyl.
“We’ve seen opioid overdose deaths in all 64 counties in Colorado,” Valuck said. “The drugs keep getting stronger and now they’re pressing fentanyl into other drugs, like cocaine, to make them cheaper. Fentanyl is now responsible for 50% of all opioid overdoses.”
The Perfect Drug
As dire as those numbers are, events like the Naloxone Awareness Dinner seek to equip as many people with the knowledge and the drug to help reduce those numbers. In addition to learning how to determine if an individual is suffering from an opioid overdose, every attendee was given the chance to receive free naloxone. A substance which Valuck refers to as “the perfect drug,” because, according to him, there are no downsides to it.
“Naloxone is a pure antagonist. There is no euphoria associated with it,” Valuck explained. “It only goes to the receptors and neutralizes the opioid. So, if there’s no opioid in the person’s system, it won’t do anything. There is no harm in administering it.”
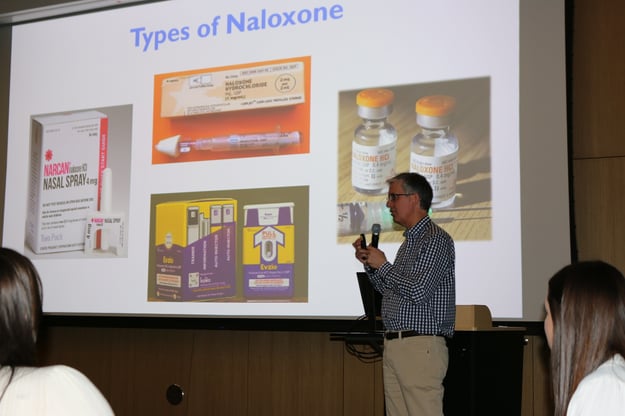
Rob Valuck, PharmD, explains how effective naloxone is at reversing an opioid overdose. |
Because of this, he encouraged the audience to err on the safe side and administer naloxone in any perceived overdose situation. The Consortium’s recently launched public awareness campaign encourages just that. The “Keep the Party Safe” campaign is targeted at young adults who might unexpectedly encounter fentanyl in a party environment. Another resource, OpiRescue, is a website and free app that provides guidelines for administering Naloxone and collects geodata about overdose response events.
“It was inspiring to see everyone gather together for the purpose of preventing lethal opioid interactions while becoming equipped with the training and medication necessary to reverse an opioid overdose,” Degagne said. “I hope this event has increased awareness about the use of naloxone and encourages others to talk to their friends and family about safe medication use.”
Naloxone wasn’t even around when J.P. and Heidi experienced their overdoses. But their parents, along with The Consortium, and concerned advocates like Ellie DeGagne, hope that events like this will equip more people with the knowledge and tools to save the lives of others.




