I met Ben Walburn at 4:00am on a slushy spring morning four years ago in a Boulder parking lot outside the house of a mutual friend, Adam. It was still dark and clouds spit little wet icicles as Ben and I huddled by our cars in the glow of headlamps, blowing steam off insulated coffee cups while trying to raise Adam via text. The plan was to exploit Adam’s birthday as an excuse for a weekend rock-climbing trip somewhere dryer and warmer – was it Escalante or maybe it was Penitente? Finally, Adam texted back: His young kids had gotten sick overnight and he had to bail. Without Adam, the trip fell apart. Ben and I made vague plans to climb together at some point, but it never seemed to come together. He was in his early 40s, I was in my late 30s, and we were both busy. Besides, it wasn’t pressing – we had all the time in the world to make it happen.
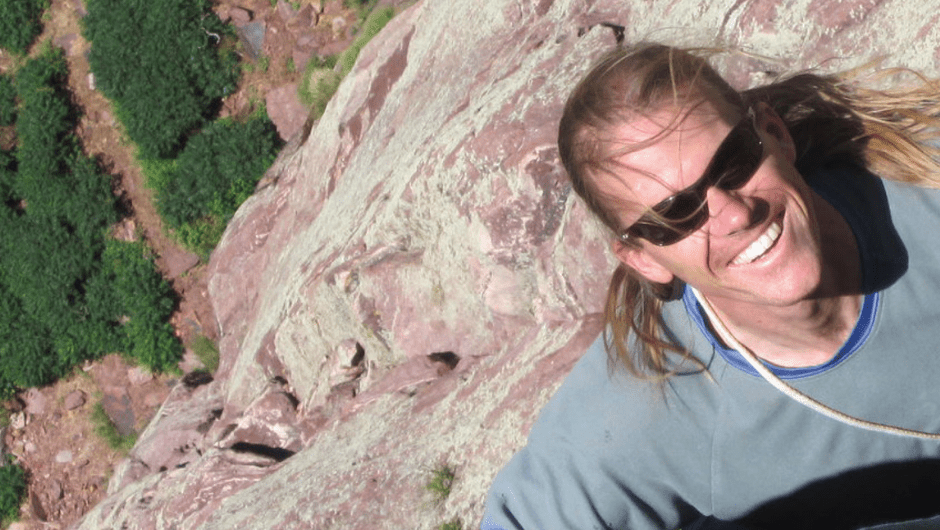
In 2017, I heard through the grapevine that Ben was diagnosed with sarcoma – a relatively rare kind of cancer that forms in soft tissue – and I got in touch to point him toward the University of Colorado Cancer Center sarcoma program, one of the few centers in the country specializing in exactly Ben’s kind of cancer. He pushed his insurance to transfer care to Anschutz and I ran into him a couple times after that, once at a climbing gym in Louisville, where it took me a minute to recognize him, bald from chemotherapy and radiation treatments; once on a sunny afternoon when he popped around a corner onto a belay ledge in Eldorado Canyon State Park; and then again in Eldo this past February at a cliff called Rincon, where Ben was climbing with an old buddy who had flown in from the east coast and his best friend from many years in Colorado.
Ben was there to say goodbye – to his friends and to this place that he loved. Because by that point it was obvious that Ben Walburn was going to die.
When Ben showed up at Anschutz, his sarcoma was already advanced. Entangled with the organs through his midsection, surgery was not an option. With treatments, he hoped to shrink the tumor enough that it could be removed, but in a scan after chemoradiation, Ben and his doctors saw that instead of shrinking, the cancer had spread to his liver, his lungs, his bones.
That February day at Rincon, I happened to be climbing with our mutual friend, Adam. As Adam and I arrived at Rincon, Ben’s group was already shoving ropes back into bags and we bantered awkwardly, nobody saying the obvious: Ben looked gaunt, fragile. How much longer did he have? Still, when we talked about the climbing route I planned to try, something Ben had done years ago, he remembered it perfectly and pantomimed the crux moves, standing on top of a boulder.

“From the left-hand crescent, kick your foot out right to the good edge and toe-in! Press the left rail and stand up to the right-hand razor blade!” he said, demonstrating with his arms and legs. I imagined how he must have looked to hikers on the trail far below, like Daniel from Karate Kid practicing wax-on and wax-off in the bow of Mr. Myagi’s rowboat. Before he left, Ben mentioned that he had a special piece of rock-climbing gear that he’d used on the route – a #1 Black Diamond Offset Stopper that fit snugly into a crack at about 2/3 height. “You place it right and that thing’s an anchor!” Ben cackled. He said that if I would stop by his house, he’d like to give the piece to me. We heard him coughing in the boulder field on the way down. His friends carried the gear.
“Isn’t life grand?” Adam said, as the sunset lit the sandstone cliff on fire.
A few days later, I knocked on Ben’s door in Lafayette. As per the etiquette in these situations, we sat in his kitchen drinking beer and telling tall tales. Like Ben’s first trip to Yosemite, when he couldn’t even get a tent site in Camp 4 and had to bail for Joshua Tree, coming back to Yosemite with just enough time for a hail Mary attempt at the route he’d spent two years training for, The Nose on El Capitan. He’d had to take whatever partner he could find, he told me, which turned out to be a Polish teenager named Robert who’d been overstaying his camping limit by hiding from the rangers in the woods with a backpack and a bicycle.
“I’m looking at the Nose, looking at this kid, and my options were one: Robert,” Ben chuckled. “We get to the top and it was great, nobody else up there, just casually in the afternoon sitting by that El Cap tree up there. The cloudscape was amazing, the view of the Valley. I proved something to myself. It felt good.” He shook his head, took another pull on his beer.
Eventually, as we both knew we would, we got around to his cancer. Ben talked about finally having to put down his beloved dog, Salsa, and about how he’d taken Salsa to a special place in Eldo, where they had shared so many days.
“When Salsa died, I was like, now I’m gonna do some trips, do some long routes,” Ben said. “May of 2017, or maybe end of April, I had just come back from my first time in Spain. I come back with a bronchial infection that lasted a long time and finally went to the doctor. He said it wasn’t pneumonia and that it would go away, but it turned out I had super high blood pressure. We followed up and I posted another high blood pressure, like 186 over 114. And I was feeling uncomfortable, started getting lower back pain, dull and droning. We decided to go in looking to rule things out with ultrasound… and that’s when we found the mass.”

Ben took a deep breath then got up and went into his back room, saying that he wanted to get the piece of gear he’d told me about. While he was rummaging around, I leaned against a doorjamb and looked across the sea of prescription bottles on his kitchen counter. Ben never married or had kids, so he could do things like that, just leave prescriptions out on the counter. I didn’t recognize most of the drugs and assumed they were painkillers and other potions for symptom management, because I knew by then that Ben and his doctors had decided against further treatment. When Ben came back, he handed me the piece of gear, a wired chunk of metal about the size and shape of a thumbnail. I thanked him and said I’d give it back after I was able to climb the route. Ben said not to worry about it – I could keep it. I was skeptical about his plan: should I really stop to shove the piece of gear into the crack like he suggested or save my energy by trying to move fast through that section?
“Take it up with you,” Ben said. “It’s nice to have it, for peace of mind, just in case.” He leaned back, running a hand across his midsection. “I can feel the tumors across here,” he said. “Sometimes it just feels like a big meal. Sometimes I can feel the lumps.”
He saw me looking at one of the prescription bottles and incorrectly assumed I knew what it was. “Yeah,” he said. “My doctor said I’m one of the first in Colorado. One of the first to, you know, use Medical Aid in Dying.” The prescription I was looking at was for a drug that could end Ben’s life.
He asked if I knew what it was like to die of cancer, or of liver failure, which is what he was looking at, and I told him that despite writing about the disease for the past eight years, I didn’t really know that much – I wrote more about science than about people – but that from what I’d heard, liver failure wasn’t the worst: You didn’t fight for breath; you felt relatively good until going downhill quickly; you knew who you were at the end. I asked what the chances were that he would use the prescription.
“I don’t know the percentage,” Ben said, thinking as he looked out the window, where the sun was shining and every so often a car drove by deeper into the cul de sac. “Probable,” he said, finally. “I don’t know the circumstances. If I’m asleep or unconscious or in pain, what’s the point? I’ll probably take it. Chances are probably pretty good.” He smiled at the piece of gear in my hands. “Anyway, it’s nice to have it, for peace of mind, just in case.”
At some point, it became obvious that Ben was all talked out and I said something about needing to go because I had to pick up dog food on the way home and cook dinner before my kids got home from practice. Isn’t life grand, I thought as I ate lasagna with my wife and two kids, our two fat Labradors under the table. Later that night, Ben texted to ask if I might want to write about him and his experience and I told him I’d be honored. Then I started thinking about it: could I really write about Medical Aid in Dying? Should I? Planning to ease into the story, I texted Ben back to see if he had time to chat a few days later, to which he replied, “The weather is calling for 44° partly sunny/cloudy and little wind…?”
This was, of course, his way of suggesting that we go climbing.
It didn’t happen. Believe it or not, the Colorado weather forecast was incorrect, and with clouds obscuring the Flatirons, we pushed climbing off to another day. Instead, we met in downtown Louisville for coffee, where Ben engaged our waitress in a “purely hypothetical” discussion about what harmless but illegal things she would do if “purely hypothetically” she found out she only had a month to live. Ben joked that he had put together a multi-sport getaway plan for robbing a bank that included running, biking, climbing, and tubing along the Boulder Creek Trail.
“I read the statistics and the only real success stories were finding it early and cutting it out. Well, we didn’t find it early,” he said, when we were alone. “Right there I’m not in a good bracket. It was pretty much then and there that I made my peace. I mean, even then you gotta try, you still hope, you can’t just give up, but I embraced the possibility of death and set out to do some things with this gift. There’s a lot of opportunity with this. I’ve learned, I’ve continued to grow, I’ve changed who I feel I am as a person. I’ve had the opportunity to heal relationships in my life, helped other people come to different understandings about me. It gives me a sense of motivation – and there’s no more need for validation.”
Ben said that what he’d really like to do is, “Go in the back of Eldo somewhere, back where I took Salsa, to drink the Koolaid,” but he’d decided against it because consuming the life-ending medication anywhere but at home is against the rules of the M.A.I.D. program and Ben didn’t want his death to make it any harder for people to use the program in the future. “Or there’s this spot off Baseline, the Dry Creek Dog Park, where all you see is the rolling field of tall grass, a rolling texture for as far as you can see, and then just boom the Flatirons rising out of it.”
Before we left the coffee shop, Ben and I made vague plans to climb together. But it never quite came together. By the time you read this, Ben Walburn will almost certainly have passed. Now, in early May, I don’t know if he will use a prescription to end his life. I also don’t know that it matters. What I do know is that we don’t have all the time in the world.
We never really did.
I used my daughter’s Dremel tool to engrave Ben’s initials in the piece of gear he gave me. I may not use it on that route up at Rincon, but it will be nice to have it, just in case. And if you find a Black Diamond #1 offset stopper cut with a “BW” stuck in a crack somewhere up in Eldo, take it with you. If you place it right, that thing’s an anchor. And as you do, think of Ben Walburn, gaunt and smiling on top of a boulder, miming moves as the sun sinks into the Divide.
Perspectives of Ben’s Providers
When I spoke with Ben, he gave his permission for me to speak with his doctors and to write about their experience as providers working with a patient using Colorado’s Medical Aid in Dying program. Despite voters’ approval of the Colorado End-of-Life Options Act in 2016, I was surprised to learn that in early 2019, both of Ben’s main doctors at CU Cancer Center had yet to help a patient pass through the program. Ben was their first. I was also surprised to learn how truly difficult it was for these doctors, personally and professionally, and how much the process forced them to reflect on their wishes for their own end-of-life experiences. Here, in their own words, is what they had to say.

VICTOR VILLALOBOS, MD
Director, CU Cancer Center Sarcoma Program
“I really like Ben a lot. He’s an incredible guy, incredibly thoughtful, and I think he’s been thinking about MAID for quite some time. He totally understands the approach – he wants to live as much good time as possible. He wants to be able to do what he wants to do. Our treatment approach has been to limit toxicity so that he can do what he likes to do for as long as he can do it and that is rock climbing. In a certain way, this isn’t new to oncology – we often sacrifice time being alive to time being comfortable. It’s new in the fact that the patient has a drug cocktail made up to die, with the intent to die quickly, but not new in trading more life for better life. Still, it was a strange feeling, writing that prescription. Most of what we do is try to help people and be safe about it. It’s a weird feeling writing a prescription for a dosage that is toxic. Looking at the doses, it’s like, wow. This process was difficult for all of us. It made me think about what I wanted for my own life. I find it very peaceful to me, to have that thought that if I had a bad diagnosis, and had implications of suffering, the idea that you would have medication available to ease that transition. Some patients don’t use that option, but even having the option is soothing.”
CLAY SMITH, MD
Program Director, Blood Cancer & BMT Program, CU School of Medicine

“Ten years ago, you could tell people with a very high likelihood that their life would not go on for a long period of time. The challenge we run into this last decade is we’re living in this age in which there is an explosion of new therapies – we’re drinking from a firehose of new treatments. And so, at least in blood cancer (less so with a sarcoma like Ben’s), it may be next month or three months or six months from now that an effective therapy could come along. It’s a wonderful time, but it makes it much more difficult to think about when to say enough is enough. It’s a conversation we’ve been having forever. But with MAID there is an active participation by the medical system in shortening a person’s life and even though I philosophically think this should be available to people, I actually decided I would not participate. What if I’m wrong and they don’t have just six months to live? Morally and ethically, I feel like it’s a person’s right, and could even consider it myself in certain circumstances, but emotionally, I don’t think I could actively write that script’ and watch someone go home knowing… On an intellectual, rational perspective, I know my thinking on this is irrational, but I don’t know how to get around that. My mind says one thing and my heart says another. What I do know is that these are the kinds of things we should be talking about all the time – the real-life stuff.”
MARTIN MCCARTER, MD
Surgical Oncologist, UCHealth University of Colorado Hospital

“Talking with colleagues, not a whole lot have experience with MAID. When the bill was passed everyone was on high alert expecting people to come out of the woodwork, and it didn’t happen. It’s on both ends – on the doctor’s side, it’s a hard conversation to have, and none of us are experienced or trained in that. And patients, in some way, are afraid to bring the topic up, I think. I talk with my residents: It’s almost like it’s un-American to do nothing. Everybody is wired to do something if it can be done, explore every last option, fight to the end. It’s a battle; it’s a war; that’s the language we use. It’s human nature not to want to die. But when you’re faced with those decisions, things change. Your perspective changes a great deal. Still, it’s a rare person who can be like Ben and say enough is enough.”
JEANIE YOUNGWERTH, MD
Director, Palliative Care Consult Service at CU School of Medicine

“When we talk about goals of care, we learn a patient’s story. We talk to them about their values, who they were before illness, who they feel they are now. When someone enquires about aid in dying, we don’t go straight into the law, we go into tell me more about wanting to learn more about this, what’s going on with you and your illness, and how is your life being affected? It’s an inquiry, a process of learning more. Ultimately, it’s about suffering, but suffering comes in so many ways and so many layers. It’s really interesting: Some things we have in our heads about what we want for ourselves, sometimes people who are actually in those positions, their minds change. Hopefully, I’ll react in the way I think I will, but I don’t think any of us can know until confronted with the reality of our own mortality. Dying well means different things to different people. Our role is to figure out what that means for each person.”