The COVID-19 pandemic had dramatic effects on all types of cancer screenings, from mammograms to colonoscopies. In the early days of the health crisis in spring 2020, screening numbers dropped dramatically as health care providers shifted their attention to caring for the seriously ill and fears of contracting the virus kept the general public away from hospitals, clinics, and other facilities.
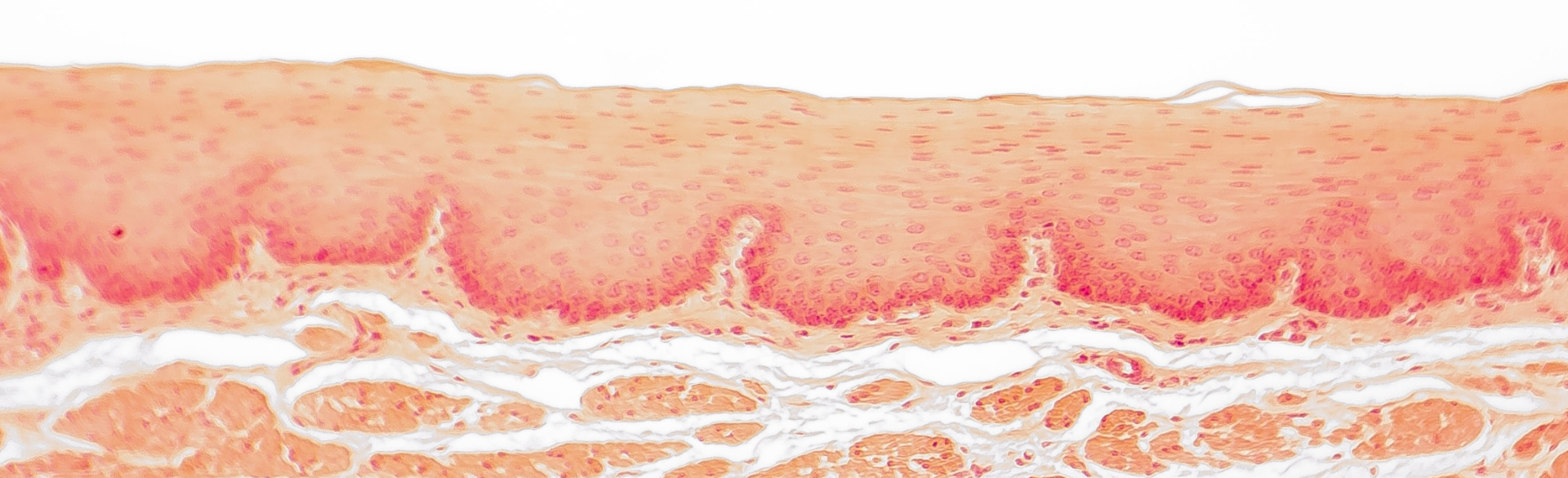
New research by University of Colorado Cancer Center member Sachin Wani, MD, director of the Katy O. and Paul M. Rady Esophageal and Gastric Center of Excellence, details the effects of the pandemic on esophageal cancer screening, looking in particular at diagnoses of Barrett’s esophagus (BE), a condition in which the lining of the esophagus becomes damaged by acid reflux, which causes the lining to appear pink with abnormal cells on biopsies. BE is the only identifiable premalignant condition for esophageal adenocarcinoma and increases the risk of developing esophageal cancer compared to the general population. Wani’s study was published October 2 in the American Journal of Gastroenterology and led by Kusuma Pokala, MD, a trainee in the Division of Gastroenterology and Hepatology and Interventional Endoscopy Section
Wani and his team analyzed data from January 2018 to December 2022, finding a significant decline in the number of BE and BE-related dysplasia (abnormal cells) diagnoses during the COVID-19 pandemic, with an almost 50% reduction in the amount of dysplasia diagnosed in the early days of the pandemic. The decrease, Wani writes, “may result in deleterious downstream effects on esophageal adenocarcinoma morbidity and mortality.”
We spoke with Wani about his research and its findings.