A new study from researchers at the University of Colorado Anschutz Medical Campus has identified a less invasive way to treat a subset of head and neck cancers that could potentially change the standard of care for patients.
HPV-unrelated head and neck squamous cell carcinomas (HNSCC) typically do not trigger immune responses and have not responded well to immunotherapies. The current standard of care for these tumors begins with surgery that can require tongue or jaw removal and other facial and oral complications, followed by six weeks of radiation with or without chemotherapy.
In a new study, just published in Nature Cancer, CU Anschutz researchers detail a different approach to treat these tumors that uses radiation combined with immunotherapy to invigorate the patient’s immune response and reduce immune exhaustion.
This approach, combined with just one cycle of the drug Durvalumab within a specific pre-operation timeframe, primes the immune system to kill most or all of the cancer before surgery. The level of success observed in this preoperative marriage of treatments is remarkable.
Study results exceed expectations
Of the 21 HNSCC patients participating in the Phase I/Ib dose-escalation study, major pathological responses or complete responses was 75%, and 89% for those in the expansion cohort who received the optimal radiation dose. And for those on the expansion cohort with MPR/CR, none of them received adjuvant radiotherapy or chemotherapy despite large tumors at presentation and none have recurred to date. Time to surgery was also a critical element in allowing response to be observed and for immune system priming to happen.
“The response in our patients to this dual-treatment protocol surpassed our expectations,” said Sana Karam, MD, PhD, corresponding author, and member of the CU Cancer Center. “By combining treatment modalities, we were able to spare our patients’ lymph nodes and prime their immune systems, ultimately resulting in a less morbid treatment regimen.”
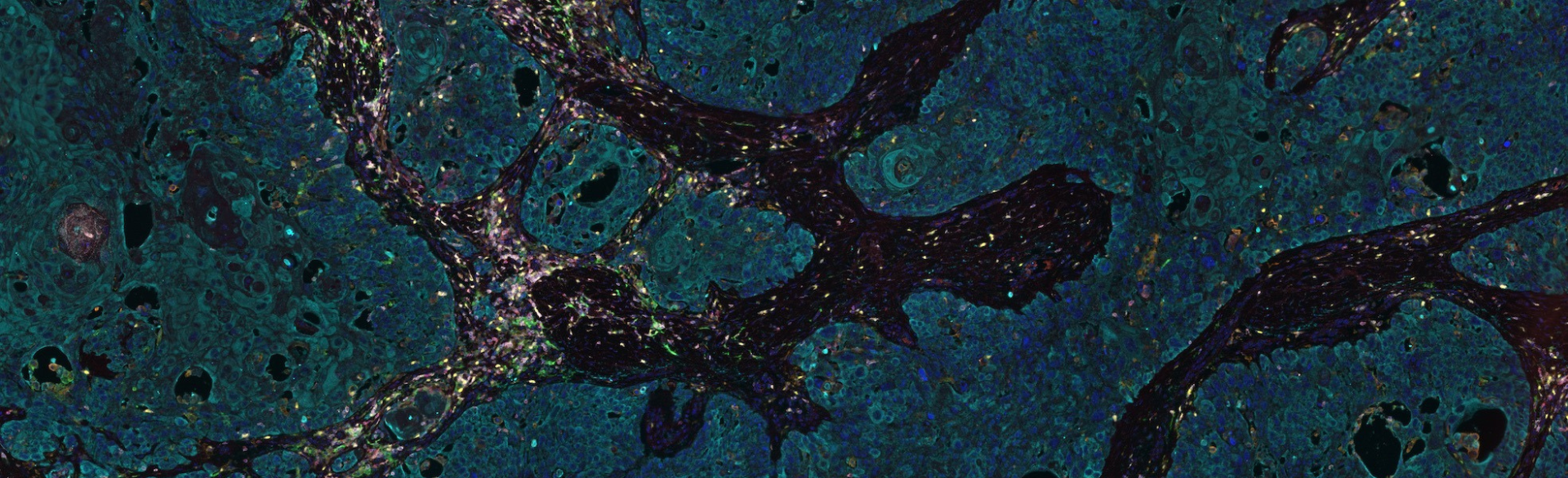
In conducting the translational analysis, CU Anschutz MD/PhD student Laurel Darragh observed a major increase in T-cell infiltration in the tumor and several biomarkers in the blood. The blood correlates could be detected preoperatively such that it was clear pre-surgery who was going to respond to the treatment. All patients went on to receive four additional cycles of postoperative Durvalumab, but those who failed the treatment did so despite the adjuvant treatment.
“Our biggest takeaway from these results is hope for our patients,” Karam said. “The response rates here are truly unparalleled, so we are hopeful that this work will lead to a significantly improved standard of care in how we treat these types of cancers.”
Researchers hope to move forward with these results to validate potential biomarkers in a larger, ongoing Phase II trial.