In the earliest days of specialized cancer care, two things often happened: either individual oncologists were burdened with the expectation to know everything, or patients were sent on treatment journeys that could involve multiple visits with multiple clinicians in multiple locations.
As the field of cancer care has grown and evolved, buoyed by tremendous strides in research and therapeutics, patients could increasingly and reasonably hope to live many years, rather than many weeks or months, after a diagnosis. A significant contributor to this hope has been the move toward multidisciplinary care.
In this coordinated care approach, teams of specialists work together and with patients to develop and continually adapt individual treatment plans.
At the University of Colorado Cancer Center, people diagnosed with cancer can receive care in multidisciplinary clinics – a sort of “one-stop shop” in which they are evaluated in one day and in one location by all of the specialists who focus on their particular type of cancer.
“At the CU Cancer Center multidisciplinary clinics, we ensure the best treatment plan by having all the various specialists – medical oncologists, surgeons, radiation oncologists, pathologists, radiologists, and many others – present, looking at all of the information, and crafting the best path forward for the patients and their families,” says Richard Schulick, MD, MBA, director of the CU Cancer Center.
Benefiting patients
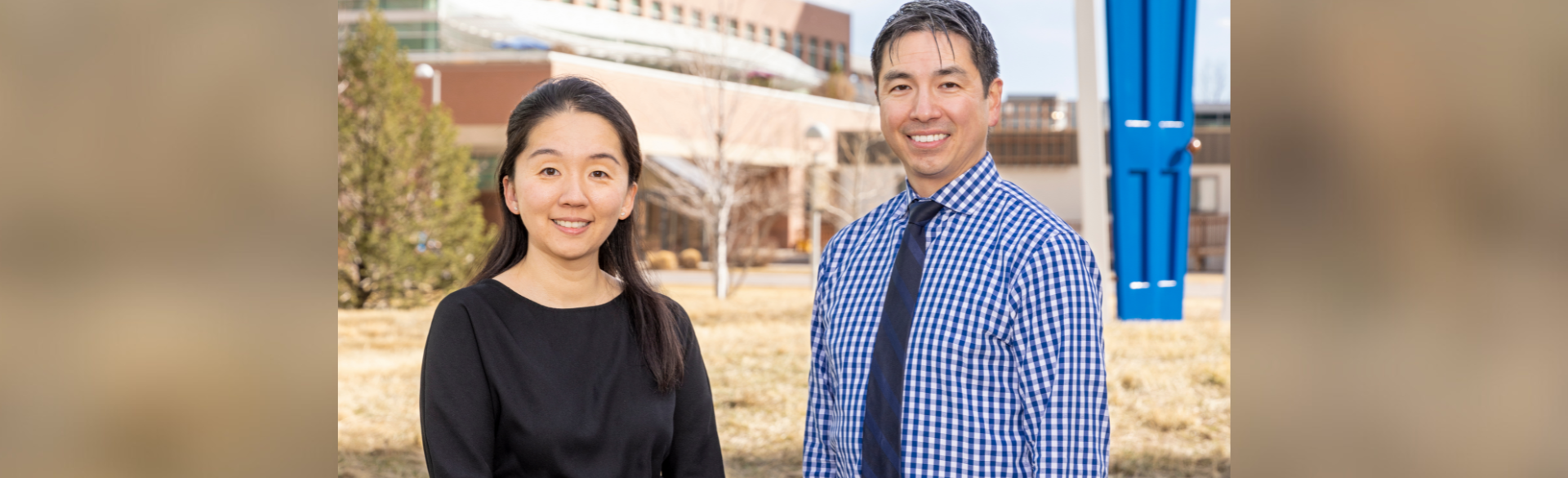
The benefits of multidisciplinary care are emphasized again and again to clinicians who work every day with patients in various stages of a cancer journey. For Christopher Lieu, MD, an associate professor of medical oncology in the CU School of Medicine, and Sunnie Kim, MD, an assistant professor of medical oncology, working with a couple in which both people are battling stage IV colon cancer has particularly highlighted the importance of a multidisciplinary approach.
Lieu is the primary oncologist for Kacie Peters and Kim is the primary oncologist for Erik Stanley. Kacie and Erik are a Denver couple who have been together for 10 years and are parents to their 6-year-old son, Nate.
→ Learn more about Kacie and Erik's story.
“I think one of the ways that Kacie has really benefited from multidisciplinary care is she’s been treated with surgery a couple of times, and this is just due to discussions of her situation with surgical specialists on the team,” Lieu says. “At the time of her recurrence, surgery was one of the first things we did. I think that ability to quickly consult with surgical specialists and have those longitudinal discussions where it’s not just a one-and-done kind of deal – having that close communication with people in different sub-specialties – has been really helpful.”
When Erik was diagnosed with colon cancer several years after Kacie, in February 2022, the disease had metastasized to his liver and was invading his ureter, as well as overtaking the sigmoid part of his colon.
As Erik’s oncologist, Kim advocated for an aggressive approach and he began a three-drug chemotherapy regimen called FOLFIRINOX. Also, because the primary tumor on his sigmoid was so large and threatening to cause a full obstruction of his colon, “we turned to the colorectal surgeon on the care team very quickly and he was able to perform a diversion. One of the interesting things with multidisciplinary care is you have the initial plan – and for Erik, that was to continue chemotherapy – but we were frequently going back to the multidisciplinary team and asking what more we can be doing for him.”
Clear channels of communication
The main goal of multidisciplinary care is to give patients the best care possible, in the clinic and in other aspects of their lives, so the approach offers an expanded umbrella of care.
While common perceptions of cancer care focus on medical and surgical oncology, multidisciplinary teams include radiation oncologists, pathologists, genetic counselors, registered dieticians, social workers, therapists, research coordinators, financial counselors, diabetes educators, and other specialists. Multidisciplinary care has grown to encompass not only the physiological aspects of cancer care, but social, psychological, and emotional needs as well.
“Something that patients especially appreciate is having one point of contact,” says Cheryl Meguid, DNP, MBA, associate professor of surgery and regional medical director of oncology multidisciplinary programs in the CU School of Medicine. “About 30% of our patients come from out of state, so it’s one trip, one facility fee, and they leave that day with a plan. It’s an incredibly patient-centered model.”
Lieu emphasizes that while multidisciplinary care teams can include several dozen experts, “the patient’s goals and values and what they want are critically important in decision making and creating a treatment plan. I think part of that is the idea that as long as we have good control of the cancer and our patients are feeling well, then that’s a win.”
“There’s always a unified plan, and I think whenever providers are communicating clearly, the patients are always going to benefit from that.”
Also, patients benefit from the clear channels of communication that are vital to multidisciplinary care. “Since we’re all talking together, patients don’t really experience doctors who are saying different things,” Lieu says. “There’s always a unified plan, and I think whenever providers are communicating clearly, the patients are always going to benefit from that.”
More effective treatments
While the focus of multidisciplinary care is providing the best treatment for patients, providers also benefit from the approach, says Wells Messersmith, MD, associate director of translational research for the CU Cancer Center and division head for medical oncology in the CU School of Medicine.
“In oncology, we often struggle to find the balance between being aggressive enough and not being too aggressive,” Messersmith explains. “And patients often have strong feelings one way or the other. Because of the weight of these decisions, we often find that making them in a multidisciplinary team approach not only gives you better decisions because you have so many people weighing in, but it helps you sleep better because you’re sharing the weight of possibly making a life-or-death call.
“Nobody has a crystal ball and sometimes we just don’t know how things are going to play out – we can only make decisions based on the best evidence we have. I think that weight can lead to burnout and stress for clinicians, so it’s much more satisfying as a provider to practice in a situation where you have other people right alongside you as you’re making those decisions.”
An aim of decisions made in a multidisciplinary team is consensus, working to ensure that each team member is comfortable with the plan and that no one provider has dominated a decision, Kim says. Many minds working together also brings innovative approaches to treatment.
Lieu notes that Kacie Peters has benefited from participation in clinical trials and received access to immunotherapy through them, a process that was initiated in part because her multidisciplinary team includes a research coordinator. And Erik Stanley has shown such a good, sustained cancer response to FOLFIRINOX that “we’ve discussed his case with liver surgical specialists on his team and we’re thinking about putting in a hepatic arterial infusion pump to try giving him chemotherapy that’s really just directed into his liver,” Kim explains.
“There’s only so much traditional systemic treatment, meaning chemotherapy, can do for him, so it’s nice that we can draw on the expertise of a multidisciplinary team to come up with more effective treatments for our patients.”