Among the biggest obstacles in studying and treating brain tumors are the blood-brain and blood-tumor barriers (BBTB). Generally, just a small amount of drug that is injected into the blood to treat brain tumors is able to penetrate blood vessel walls and accumulate in the brain.
Glioblastoma, one of the most aggressive and devastating brain tumors in adults, can hide and grow behind the BBTB. Even when treatment incorporates nanoparticles to carry a drug to the tumor, those nanoparticles still can have a hard time penetrating the BBTB.
However, a University of Colorado Cancer Center researcher, in collaboration with colleagues from Northwestern University, has developed a lipid nanoparticle that is highly efficient in penetrating the BBTB and accumulating in glioblastoma.
Dmitri Simberg, PhD, an associate professor in the Skaggs School of Pharmacy and Pharmaceutical Sciences and co-director of the Colorado Center for Nanomedicine and Nanosafety, recently published significant research findings that show great promise in guiding the development of indocarbocyanine lipid nanoparticles (ICLs) that can deliver anti-cancer therapies to tumors in humans. This work was done in collaboration with Irina Balyasnikova, PhD, of Northwestern University.
“Based on what we’ve learned so far, we plan to use nanoparticles to understand more in general about how they can accumulate in brain tumors,” Simberg says. “We also are working to incorporate cancer drugs, using lipid nanoparticles as cancer drug carriers, targeting just the tumor.”
Targeting tumor cells
This research is part of broader nanoparticle research recently funded by a five-year National Institutes of Health grant to support research into how nanoparticles accumulate in brain tumors, and also how attaching drugs to nanoparticles may prolong the effectiveness of cancer therapies.
"A premise of this research is to enhance accumulation in the tumor, while limiting the actions of the drug all over the body,” Simberg explains. “The more we’re able to deliver drug specifically to tumor cells, the more we can spare healthy tissues.”
Simberg and his co-researchers worked with ICLs formulated in a PEGylated lipid nanoparticle (PLN). Lipids are good at migrating and spreading through tissues, so a goal is to inject them into the blood so they can penetrate a blood vessel wall and reach every possible cell in a tumor, delivering a drug payload.
“Because ICLs can move around in tissue better than standard lipids, once they get out of a blood vessel, they can rapidly spread all over a tumor and reach brain-invading cells that break out of the tumor,” Simberg says. “They can reach cells that other therapies can’t.”
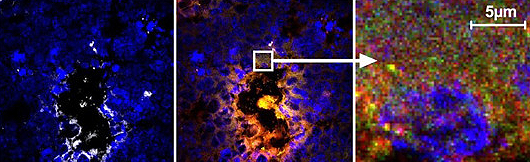
In glioblastoma animal modeling research, PLN-formulated lipids were injected into a subject and their migration was tracked over time, which was facilitated by the lipids’ fluorescence. An hour after injection, over 82% of the tumor’s extravascular area was positive for the lipid fluorescence in the group that received the PLN-formulated ICLs, compared with 13% in the group that received standard liposomal treatment. Forty-eight hours later, PLN-formulated lipids were present in a majority of tumor cells.
Carrying drugs to brain tumors
One interesting aspect of the research is that the particular lipid nanoparticle used became smaller after it was injected into the blood, which may have helped it get through the blood vessel wall and to the brain tumor cells. Further research will investigate this phenomenon, including looking at how the lipid nanoparticles interact with the protein in plasma.
The next phases of research also will continue exploring how lipid nanoparticles can carry drugs to brain tumors.
“There are a good number of drugs that can be linked to a lipid,” Simberg says. “There is something called a cleavable bond, meaning the lipid and drug are linked together when they’re injected but once they get inside tumor cells the drug can be released."
Simberg and Balyasnikova also plan to create a library of lipids with different structures to see which ones work better for delivering specific drugs to specific tumor cell types “because we want to see how we can improve selectivity of drug delivery,” Simberg says. “There’s potential for a whole range of different treatments that can combine with a nanoparticle approach.”