Combining targeted therapies known as tyrosine kinase inhibitors (TKIs) can be an effective way to treat a mutation-driven form of lung cancer in cases where tumors develop resistance to treatment and where cancer has spread to other parts of the body, a University of Colorado Cancer Center member reports.
“This combination has not been studied very well before, and it really has shown some impressive results,” says Tejas Patil, MD, an assistant professor in the CU Division of Medical Oncology.
Patil was lead author of a paper on the study published recently in JTO Clinical and Research Reports, a journal of the International Association for the Study of Lung Cancer. Several of his division colleagues were co-authors.
Lung cancer is the leading cause of cancer death, accounting for almost 25% of all cancer deaths. In Colorado, the American Cancer Society predicts there will be 2,660 new cases of lung and bronchus cancer diagnosed in 2024 and 1,290 deaths.
Non-small cell lung cancer (NSCLC) represents about 85% of all lung cancers. About 45% of patients with NSCLC have specific mutations called oncogenes that cause a cancer cell to grow, Patil says.
A major clinical challenge
“For many of these patients, if we block the oncogene, we can control cancer growth. Many of these patients don’t get chemotherapy or immune therapy. They just go on targeted therapies that have been engineered to target the very specific mutation that their cancer has,” he says.
The targeted therapies used in such cases are TKIs. They block growth pathways that help cancer cells grow and divide. “But these patients will almost inevitably develop resistance to therapy at some point,” Patil says. “It’s a major clinical challenge.”
His paper focuses on one category of resistance to TKI therapies called acquired MET resistance, which accompanies several different oncogenes that each have individual targeted therapies. “The resistance across all of them seems to be very similar,” he says. “About 15% to 20% will have this MET-mediated mechanism to resistance. And you can target the MET pathway with its own unique targeted therapy.”
Patil and his colleagues set out to assess the effectiveness and safety of combining MET-specific TKIs, such as crizotinib, capmatinib, or tepotinib, with “parent” TKIs targeting individual oncogenes as a way to overcome acquired MET resistance in patients with metastatic NSCLC driven by oncogenes.
Their study involved 83 patients at the CU Cancer Center and two other academic cancer centers with metastatic oncogene-driven NSCLC – 41 of them with acquired MET resistance and 42 without resistance. The MET group continued on a parent TKI with a MET TKI added. The non-MET group also stayed on a parent TKI with chemotherapy added.
Most respond to therapy
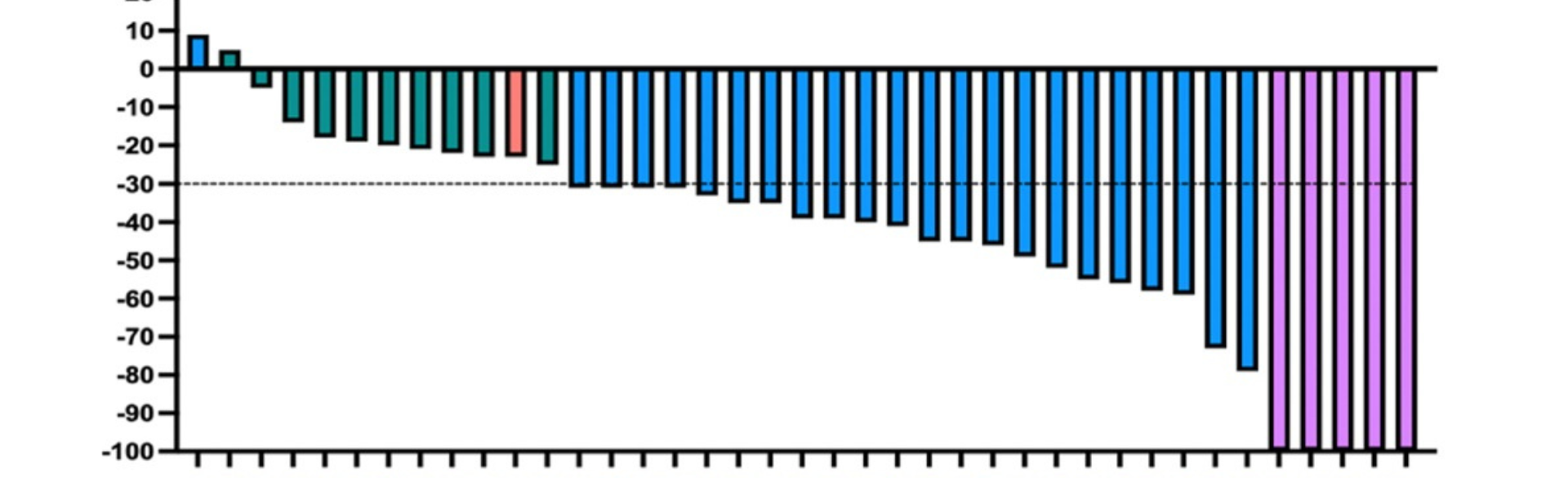
What Patil and his team found was that all but two of the patients in the MET group responded positively to the combined treatment, with their cancer shrinking to various degrees, and five of the 41 patients had “a complete response, with absolutely no cancer visualized after starting this combination treatment,” he says.
“The important message is that most patients who start this combination treatment will have a response to therapy, and that’s great,” he says. “The combination of parent TKI and MET TKI is also well tolerated and does represent an alternative to chemotherapy in patients who do have a MET-mediated mechanism of resistance.”
The paper says further research is needed to better understand how cancer cells use MET signaling to resist TKIs, and also to find the diagnostic tests that can best predict which patients will most benefit from the multi-TKI treatment approach. Patil says he’s working with Amy Young, MD, PhD, an assistant professor of pathology, on a follow-up study on MET-mediated resistance.
Patil says the CU Cancer Center’s Biostatistics Core performed the statistical analysis for the project. “This couldn’t have been done without their support,” he says. Other CU Anschutz Medical Campus resources played important roles, and the cancer center provided a support grant.
Other CU Cancer Center members who co-authored the paper include Paul Bunn, MD; Erin Schenk, MD, PhD; and Ross Camidge, MD, PhD.
Diagram at the top shows the response of 41 lung cancer patients with acquired MET resistance who received a combination treatment that included MET tyrosine kinase inhibitors (TKIs). Each vertical bar represents an individual patient, and the numbers at left indicate percentage of response to treatment. The longer the line, the greater the response to treatment. The diagram shows that five patients (at right) had a complete response to treatment, with no cancer visualized. Diagram courtesy of Tejas Patil, MD.