Benjamin Brewer, PsyD, is a University of Colorado Cancer Center investigator and health psychologist at the UCHealth University of Colorado Hospital Bone Marrow Transplant Program, providing mental health and counseling services for highly immunocompromised patients who are often in the hospital four weeks or more. For these patients, catching COVID-19 could be deadly and the climate of uncertainty adds another layer of stress to an already challenging experience. Here we talk with Dr. Brewer about his patients’ new worries and about how our health system is adapting to meet the mental health needs of cancer patients during COVID-19.
CU Cancer Center: If you had to pick one new concern you see in your patients related to COVID-19, what would it be?
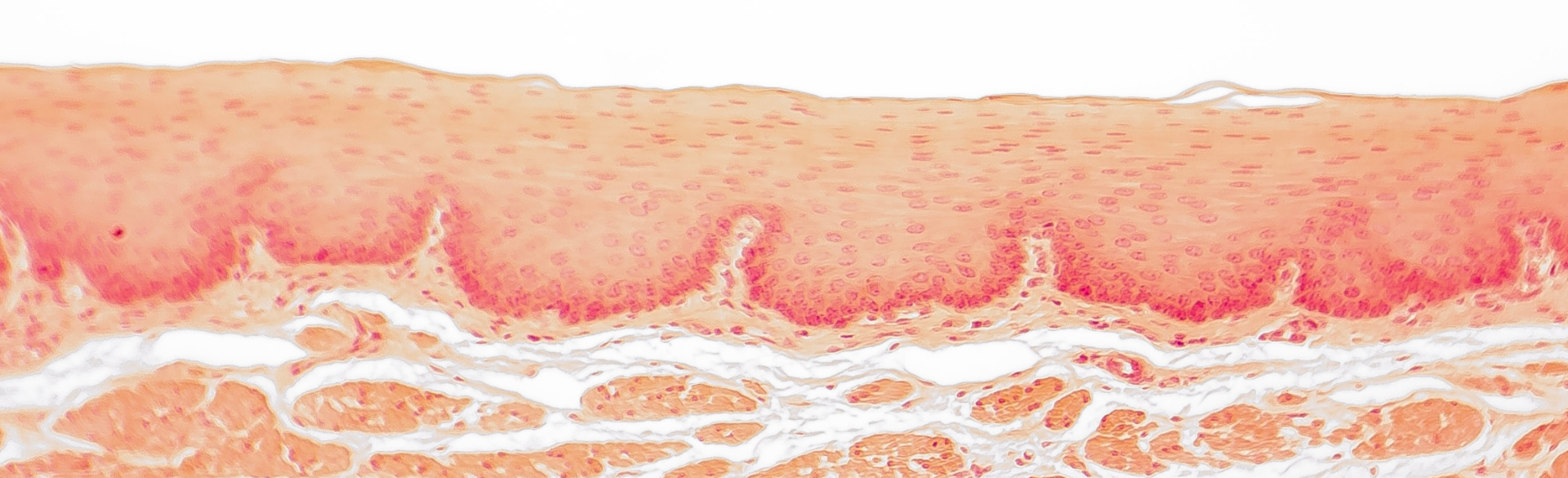
Brewer: Obviously, patients are really terrified of catching the virus, and understandably so – most of my patients are profoundly immunocompromised, either due to their disease or to the need to suppress patients’ immune systems post-bone marrow transplant. These patients are arguably some of the most vulnerable people in the whole hospital system. But even more than that, a lot of my patients are worried about what would happen now with normal problems – will we have the hospital capacity to take care of them? They’re worried that if they were to have complications like sepsis or an infection or problems that require an ICU bed, that space wouldn’t be available.
CU Cancer Center: Those fears sound like more than enough, but we’re guessing that’s not the end of it?
Brewer: Another area of increased stress is the fact that most hospitals aren’t allowing visitors. Some of my patients are in for a month or more, and families not being able to visit is really hard. People want to monitor them, push them to eat, etc. Or there’s people who say, “My partner really will not do well if I’m not there!” The toughest thing in the hospital is that isolation. Also, visiting is one thing that people could control – one thing they can do for their loved ones during treatment. Now, just when people are looking for areas of control during COVID-19, that control is taken away.
CU Cancer Center: And some families go way out of their way to be close during a patient’s stay…
Brewer: Transplant is such a big event – their family wants to be there with them. This is especially hard for our patients who come from out of state or from rural parts of Colorado. Often families will find a way to stay locally during treatment, taking time off from work and changing up their lives so they can be here. Now all those plans have to change, too.
CU Cancer Center: Right, and having an involved caregiver is so important for these patients!
Brewer: Without a caregiver when they go home, these patients don’t do well. That’s why for a transplant, we require a caregiving plan – for an allogeneic transplant you need a designated caregiver for two-to-three months after a patient leaves the hospital. We’ve had many caregiver plans disrupted by travel restrictions, illness, or the caregiver suddenly needing to provide childcare due to the closing of schools. Due to this we’ve had to keep some patients stuck in the hospital that we would like to discharge. Now with covid, when we’re doing these plans pre-transplant, we’re requiring second- and third-line backup plans. What if a caregiver can’t travel here like they planned, or what if the caregiver gets sick? If someone doesn’t have a second line caregiver, it can mean we keep them in the hospital. And this is right at a time we want to get people out of the hospital instead of keeping them in there.
CU Cancer Center: How do you see patients reacting to these worries?
Brewer: In a lot of different ways, actually. A lot of newly diagnosed cancer patients say they can’t afford to be sick right now because they don’t have time to be sick due to their other responsibilities. During the pandemic, that’s amplified. Patients feel like they need to be doing things to support their families. Anxiety is amplified, too. I talked with a woman newly diagnosed with AML and she said something like, “I had to get AML the month we’re having a pandemic!” She said that dealing with cancer is one thing, but dealing with cancer while dealing with all the worries that come with covid is another. On the other hand, I’ve had a number of patients who’ve said to me, “Heck, I have to be mostly isolated for 3-6 months of my life, and it just feels like everyone is in solidarity with me – like the whole world has to have a bone marrow transplant today!” I know they’re using humor to mask real worries, but some of my younger patients joke that their fear of missing out is much less now that there’s nothing to miss out on…
CU Cancer Center: Do these worries create their own problems?
Brewer: Certainly. We’ve had a number of patients develop psychosomatic issues – a psychosomatic cough or diarrhea, or stress-related problems like muscle stiffness and headaches. People are having sleep issues, anxiety, or symptoms of panic like feeling their heartbeat or sweating. And when we dig down, the root is pervasive chronic stress from covid in the context of their cancer. It’s not just patients but the whole team, the whole staff – overall, all of us are more anxious.
CU Cancer Center: It sounds like we could all use mental health care right now…
Brewer: When I call to set up virtual visits, patients are really relieved that they can have behavioral health visits without needed to come into clinic, where they are afraid of infection. Everywhere, patients are really grateful for mental health care, even for phone visits. We’re also suggesting that health professionals get mental health care, too. We don’t want our healthcare providers to burn out now when we need them most. My colleague, Dr. Becky Hunter has been heading up our staff support and this is a large project and has been well utilized by our team.
CU Cancer Center: So what do you tell cancer patients right now? How do you speak to these anxieties?
Brewer: Well, first, our bone marrow transplant unit has always had to be really careful with infection. Many of our patients are used to wearing masks at times, and are used to some level of social distancing as these are recommendations of our program during normal times. We have not had a flood of BMT patients with COVID, probably due to this approach before the virus was even apparent in the population. Because we’re always been aware of infection, in some ways, our unit probably decreases the chance of catching the virus. Also, I’ve been really impressed with how everyone in our team and the hospital has helped prepare. For example, we converted outpatient visits to virtual – within one week, we got everything flipped. We also started virtual support groups. Elective surgeries are being postponed, and we’re also postponing less pressing transplants so we have good capacity to handle the urgent stuff. The facts are actually reassuring: We’ve diverted a lot of other procedures to make space and I’m confident we’ll have the resources we need to treat these serious cancers. My team is very dedicated to making things work for all of our patients and I think patients have been reassured by this. Our leadership has done a remarkable job with all of the transitions and coordination. Psychologically, we’ve sort of ranked COVID as the top concern, but for my patients, cancer and their transplant are still the most pressing problems. I’m trying to help them focus on managing anxiety and health behaviors to support their cancer treatment. By the time a patient diagnosed today finishes their treatment, maybe we’ll all be ready to get back to our lives – we’ll all come through this together.