Squamous cell head and neck cancers — cancers that develop in the outer layers of tissue in the oral cavity, throat, larynx, and sinonasal cavity — are the sixth most prevalent cancer worldwide. The five-year survival rate for this type of cancer is 40% to 50%, with a worse prognosis for patients with advanced disease.
Treatments for squamous cell head and neck cancers have been slow to develop, largely because there are no animal models directly comparable to this type of cancer in humans. However, new research by University of Colorado Cancer Center researchers Mary-Keara Boss, DVM, PhD, and Dan Regan, DVM, PhD, both of the Flint Animal Cancer Center at Colorado State University in Fort Collins, shows that this type of cancer in dogs has significant biological overlap with the disease in humans, making dogs with naturally occurring head and neck cancers good subjects for clinical trials of new treatments, including immunotherapy.
“I'm a veterinary radiation oncologist, and when I got to CSU, I was introduced to Sana Karam, who's a radiation oncologist for human patients,” Boss says. “We both treat patients with head and neck cancer, and we share an interest in studying radiation and immune effects. In talking with Sana about what we could do to collaborate to treat our cancer patients, and how we could translate things across species, we realized that there's a big gap between what we can do in the lab versus in-human clinical trials. We wondered, could dogs fit an unmet need for studying this cancer?”
Setting the baseline
Karam, MD, PhD, a CU Cancer Center member, is another author on the paper published in January in the journal Frontiers in Oncology. As a first step toward using dogs as a surrogate for human head and neck cancers, the researchers looked to characterize the baseline immune landscape of naturally occurring oral cavity cancers in dogs. They also were able to demonstrate the presence of immunotherapeutic targets in the tumors that could be valuable in future immunotherapy trials.
“There's nothing like this in the literature,” Karam says. “Not only did Boss and Regan subset the tumors by what's inside them, but also their functionality. That's where the strength of this lies. For clinical trials, you may be able to categorize patients — canine patients or human patients — based on these subsets.”
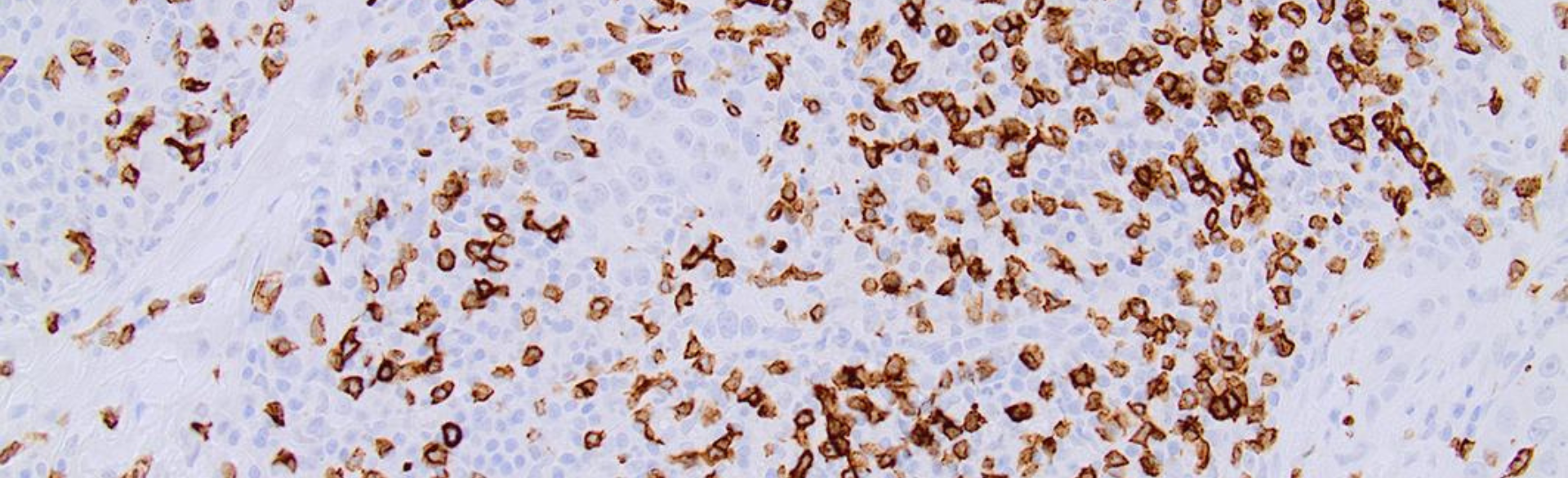
Boss and Regan used archived tumor and normal mucosal samples from 34 dogs to put together their analysis, comparing each type of tissue sample to identify the unique qualities of oral cancer cells. They found that, like human oral cancer cells, the canine cells contain a heterogenous tumor immune microenvironment with a high number of CD3-positive T cells.
“We recognize that this is a retrospective analysis from archive samples, but now that we understand from those what the landscape looks like, we can enroll prospective patients in trials,” Boss says. “We looked at different markers that we could investigate for different immune modulation approaches.”
Hot and cold tumors present different targets
The researchers also found a mix of “hot” and “cold” tumors in the archived samples — hot tumors that contain a high number of T cells and are more easily able to mount an immune response, and cold tumors that have few to no T cells and aren’t as accessible to immunotherapy, which boosts the body’s natural immune response.
“T cells were the most common immune cell throughout the tumors, but when we looked at how they were distributed, 80% of the samples were pretty infiltrated, with plenty of T cells around the tumor,” Boss says. “But we did see that 20% had more of that cold microenvironment. While there's a good amount of inflammation and markers of antitumor responses in these tumor samples, there's also the potential for there being suppressive activity. That means we could potentially be doing better with treating and controlling these cancers if we were able to modulate or really boost immune responses.”
Looking at other cancer types
Boss and Regan are currently working on a similar study of dogs with sinonasal carcinoma and will be performing a comparative analysis with human samples through collaboration with Karam, hoping to establish the baseline tumor microenvironment and to re-evaluate that microenvironment as the animals go through different clinical trials.
“There is a collective effort at the Flint Animal Cancer Center to look at a number of different canine tumor types that might be good translational models for human tumor types,” Regan says. “Our overall hypothesis was that there would be similarities to the immune landscape of the same human tumors. It was great to have Dr. Boss come in with slightly different expertise, being a radiation oncologist, and have an interest in a different tumor type that we really weren't working on at the time.”
Image: This photomicrograph shows immunohistochemically labeled CD3+ T cells infiltrating a canine oral squamous cell carcinoma tumor.