“Over-performing.” It’s a label that reflects years of effort and dedication by University of Colorado Department of Medicine, Division of Hematology and CU Cancer Center faculty and staff in the field of stem cell transplantation.
Only 11 centers of allogeneic stem cell transplantation – using stem cells from a source other than the patient – have been classified as "over-performing” out of 178 centers nationwide in the latest annual evaluation by the Center for International Blood and Marrow Transplant Research (CIBMTR).
The CIBMTR evaluation is based on one-year patient survival rates after allogeneic stem cell transplants as compared to predicted survival rates derived from various measures of risk among each transplant center’s patient population.
In the case of the stem cell transplant program at UCHealth University of Colorado Hospital, the actual survival rate is 79.3% versus a predicted rate of 72.7%.
“We like the recognition, but even if we weren’t on the list, I’d still say we were the best,” says Jonathan Gutman, MD, professor in the Division of Hematology, Director of the Allogeneic Stem Cell Transplantation Program and a CU Cancer Center member.
He says the program has been growing steadily for several years and now performs about 90 allogeneic stem cell transplants each year. Gutman gives credit for the program’s success to “an absolutely fabulous team.”
Outliers on cord blood
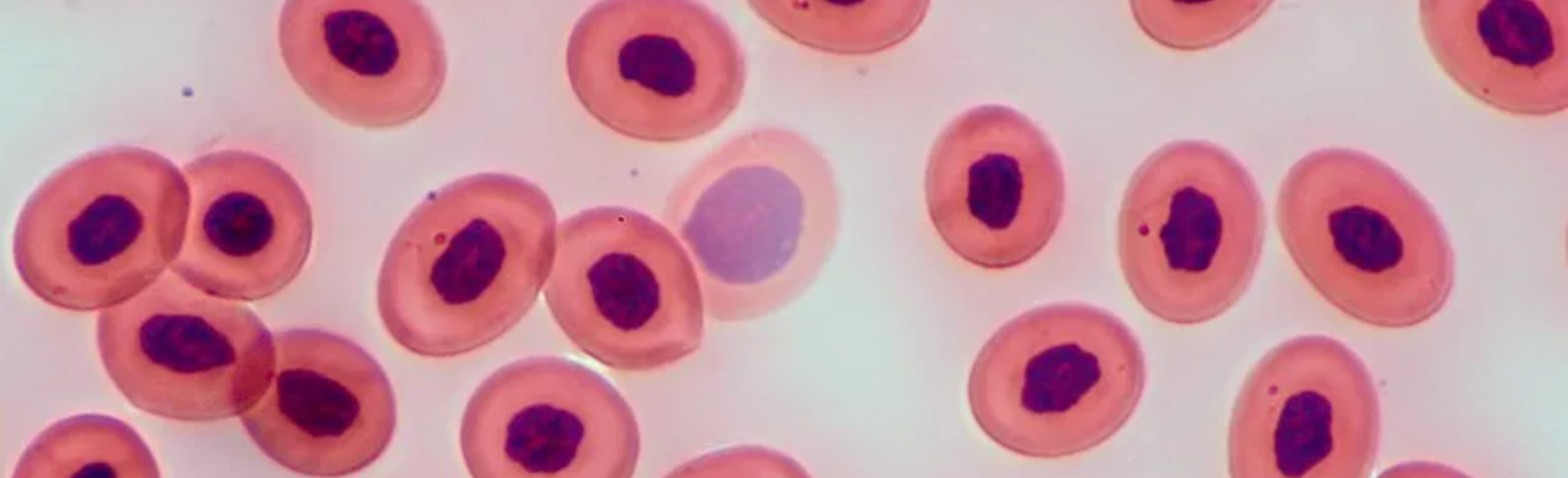
A stem cell transplant, also called a bone marrow transplant, replaces stem cells in a patient’s bone marrow to grow new, healthy blood cells in a patient with a blood cancer. The body needs enough healthy stem cells to produce blood cells and platelets in the bloodstream.
Stem cells to be transplanted are sometimes collected from a patient’s own body before chemotherapy or radiation treatments, and then reinserted after treatment. Otherwise, in an allogeneic transplant, the transplanted stem cells come from elsewhere. They can be collected from the blood of a donated umbilical cord or from a donor’s bone marrow or blood.
Gutman says he and his colleagues have “been outliers historically” in emphasizing cord blood as a donor source for stem cell transplants, “in part because we know we get really good outcomes from it.”
Cord blood is banked for public use at storage centers worldwide. Research published in 2020 by Gutman and others showed that recipient patients receiving cord-blood transplants did as well or better than patients receiving transplants from matched siblings.
Not just a number
Beyond the science, skill and experience involved, at the core of a successful stem cell transplantation program is great team communication with patients, Gutman says.
“The most significant job that you have as a transplant physician is your initial conversation with patients about what is a transplant, and is it right for them, because it is a very complicated procedure fraught with risk. Whether it's right or not for people is often not a black-and-white question. There’s a lot of grey in that decision, particularly with older patients who might have other medical issues and alternative therapeutic options,” he says.
“For any patient, this is a deeply personal experience, and we greatly value the individual attention we give to our patients as we work through that. You know, patients are not just a number as they come through this institution. Culturally, we want to keep it that way.”
“It takes a village to do a transplant,” Gutman adds. “It’s nurses, it’s social workers, it’s psychologists, it’s doctors, it’s the palliative care team, it’s coordinators, it’s pharmacists, it’s the insurance team. We have a wonderful team that provides great care to patients, and this recognition is a cherry on top.”
Information on CIBMTR’s methodology can be found here.



.png)