When a blood cancer patient needs a bone marrow transplant, there are four common donor sources: A matched related donor (sibling), a matched unrelated donor (from a donor database), a half-matched donor, or umbilical cord blood. Of course, there are plusses and minuses to each approach, but consensus has generally ranked a matched sibling first, followed by a matched unrelated donor, with cord blood and half-matched donors reserved for patients without either of the first two options. Now a University of Colorado Cancer Center study based on a decade of research and treatment may reshuffle this list. In fact, the comparison of 190 patients receiving cord-blood transplants with 123 patients receiving transplants from the “gold standard” of matched sibling donors showed no difference in survival outcomes between these two approaches, with significantly fewer complications due to chronic graft-versus-host disease in patients receiving transplants from cord blood.
Jonathan Gutman, MD
“Our cord blood patients were doing as well as patients receiving transplants from matched siblings, and in selected populations cord blood patients were doing even better. Our program at CU Cancer Center is somewhat unique in its emphasis on cord blood as a donor source for stem cell transplants and this study is an affirmation of why we do what we do here,” says Jonathan Gutman, MD, CU Cancer Center investigator and director of the allogeneic stem cell transplantation program at UCHealth University of Colorado Hospital.
In addition to showing a decrease in the chance of graft-versus-host disease, which develops when a transplanted blood system attacks a patient’s tissues, the study shows a slightly lower rate of relapse in these patients undergoing transplant with cord blood.
“Especially with younger, fitter patients who we can hit harder in the transplant process, we have strong hints here that cord blood may be actively better in terms of reducing both graft-versus-host disease and relapse,” Gutman says.
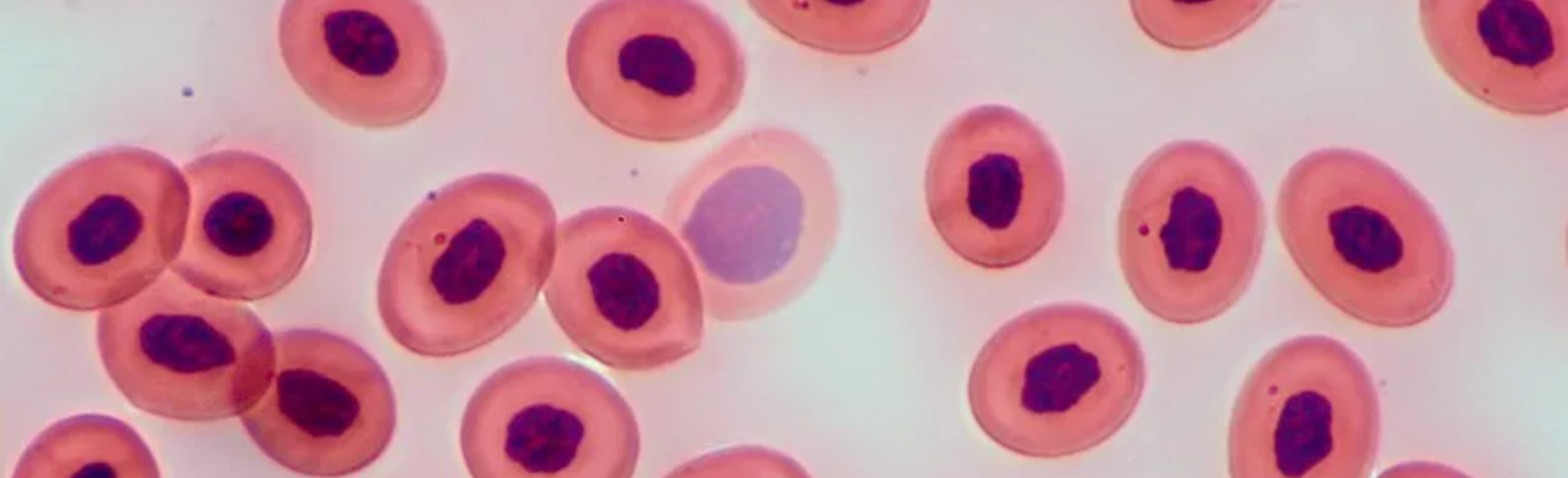
Umbilical cord blood, which is banked for public use at designated centers around the world, is rich in stem cells, which can repopulate a patient’s blood system. Because these umbilical cord stem cells are more “basic” than adult blood cells, they require a lower degree of match than blood cells from an adult donor. However, one challenge has been obtaining enough of these cells to perform a successful transplant.
“It turns out that for adults, it’s very hard to find a single cord blood unit that meets the parameters we know need to be met in terms of size. To overcome this barrier, we often use two units from different sources,” Gutman says. Also, research at CU Cancer Center and elsewhere is developing techniques to expand small samples of banked cord blood to the volume needed for transplant.
“We think there are important advantages of cord blood, especially with respect to graft-versus-host disease,” Gutman says. “Previously, we’ve taken a position recommending cord blood over matched unrelated donors, and now we show that cord blood may even out-compete the gold standard of matched sibling donors.”