It seems that there’s still a prevalent mindset of, “Oh, they’re kids, the weight will just come off.” How do you address this?
That is something we hear a lot, that they’re so much younger and have their whole lives ahead of them; do we really want to make permanent changes? But these changes are durable and safe, and they’re durable and safe over a lifetime. We also hear arguments that kids should just be better about diet and exercise because they’re younger and more active. But once adolescents reach that BMI of 35, it just gets so much harder to do it through diet and exercise. And this isn’t even taking into account the complicating factors of socio-economics and environment.
Denver Health also has a multidisciplinary program called Healthy Lifestyles Clinic for children 2 to 17 who are working on those behavior changes. They are supported by a medical provider, a registered dietitian, a behavioral health consultant and a health coach, and the Bariatric Center has a close working relationship with that program. As a result, patients and families have the option of selecting which level of intervention best meets their needs, and complicated patients who may benefit from surgery due to comorbidities or not making good progress can be connected directly with the Bariatric Center team.
You mentioned that overweight and obesity disproportionately affect children who are from underserved and uninsured populations. How will you address these issues of access to bariatric surgery?
We know that adolescents as compared to adults who have insurance claims submitted for bariatric surgery are more likely to be denied. So, we already have a plan for getting standardized appeal letters together to be able to fight to get it across the finish line. And we already have established a precedent to fund bariatric surgery for our patients who are enrolled in both the Denver Health Financial Assistance Program and Colorado Indigent Care Program.
Bariatric surgery seems like a significant life choice for someone as young as 15. Why is it necessary?
We know that the obesity epidemic is affecting children as well as adults and we know there are the same disparities by race and insurance status in terms of obesity in children and adults, meaning children from underserved communities and uninsured children are more likely to be obese or severely obese compared with their insured, white counterparts.
And while there are certainly genetic predispositions, the factors affecting obesity and severe obesity also include family stability, access to healthy food, access to parks, stress levels, employment, and other socio-economic factors. Obesity is impacting certain populations more than others. And, unfortunately, it is precisely these communities that are the least likely to have access to affordable, high-quality bariatric surgery.
We also know that obesity and severe obesity, over the long-term, can cause very serious problems like diabetes, high blood pressure, sleep apnea, joint problems, depression, and other issues. For adolescents, bariatric surgery can have a preventative effect. We can help prevent diabetes, for example, from ever developing in the first place. Once we recognize the pattern, the earlier that we can intervene to break the cycle, the more protective the effects of weight loss will be.
Bariatric surgery isn’t just about the surgery; it requires holistic lifestyle changes. How do you help ensure adolescents make these big changes?
It’s interesting, because over the last year we’ve had a lot of discussions within the bariatric team about moving the lower age limit for surgery from 21 to 15. Some of the team members have noted that our 21- to 25-year-old group can sometimes struggle with the commitment and program requirements.
But at the end of the day, a lot of 21- to 25-year-olds have started life on their own, they’re not living with family and may not benefit from as much family support, whereas a 15- or 16-year-old in general is going to have that family support through the process, have someone driving them to appointments. And there are no data suggesting that adolescents are any less likely to receive and process the information differently than our older patients.
There is a certain stigma about it not being a good idea for adolescents, and we are seeing that when adolescents are ultimately referred for bariatric surgery, their BMI is much higher. For adults to receive bariatric surgery, the average BMI is 42, 43, but the average BMI for adolescents is 55. We know that when you get to 35 BMI, it’s unlikely that you’ll lose weight through diet and exercise alone, and that’s when the risk for diabetes really increases. So, that’s when we want to intervene.
There’s a lot of preparation that happens before and after bariatric surgery. What will this process be like for adolescents?
We’re going to approach this in a multidisciplinary way. It will start with a family’s pediatrician initially broaching the idea, and then early in the process I’ll see them for an introductory visit. The children and families will work with child psychologists, social workers, dietitians, so by the time they are ready for surgery we’ll have a comprehensive plan in place.
Obviously, some parents are not going to be on board or want this for their children, but others most certainly are. Most people know at least one person who’s had it, so it’s a lot less scary and mysterious, and bariatric surgery itself has become much more standardized and less risky. That’s actually part of the accreditation process, showing outcomes data and showing that as a facility your outcomes are outstanding.
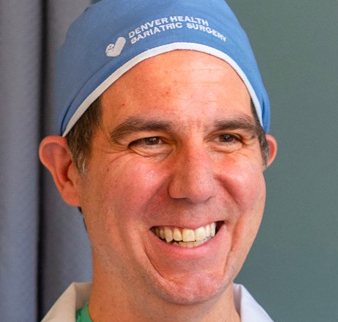
I think gone are the days when you would just go to any hospital and receive bariatric surgery from someone who only does three or four a year. Patients are much more empowered and they know they can expect this level of specialization. We’ve identified and partnered with two of our pediatric surgeons, Annie Kulungowski, MD, and Denis Bensard, MD, and we’ll spend the next six months credentialing and proctoring them to standardize our care with our adult best practices.
We’re also partnering with liaisons in pediatrics, child psychology, dietetics, and social work so children and their families can receive truly multidisciplinary care. We’ll be the only bariatric surgery center in Colorado that offers both adolescent and adult surgery on the same campus and we’re excited to be able to serve our community in this way.




.png)
.png)