Lymphedema — a buildup of extracellular fluid that occurs when the body’s lymphatic channels are obstructed or missing — can be an unfortunate side effect of surgery for breast cancer. A new device in use at the University of Colorado Department of Surgery can help detect lymphedema early, before it causes serious problems.
“The most common reason lymphedema develops after breast cancer surgery is secondary removal of axillary lymph nodes to manage cancer metastases,” says Katie Egan, MD, assistant professor of plastic and reconstructive surgery. “That creates an obstruction to the normal lymphatic clearance in the body, so lymphatic fluid can back up distal to that area. Patients get lymphedema typically in their arms or upper extremities, but sometimes in the breast and the chest wall as well.”
Lymphedema can cause decreased quality of life and decreased function, Egan says; patients are also at increased risk for infection, cellulitis, and sepsis, and can even develop a secondary cancer called angiosarcoma.
New detection tool
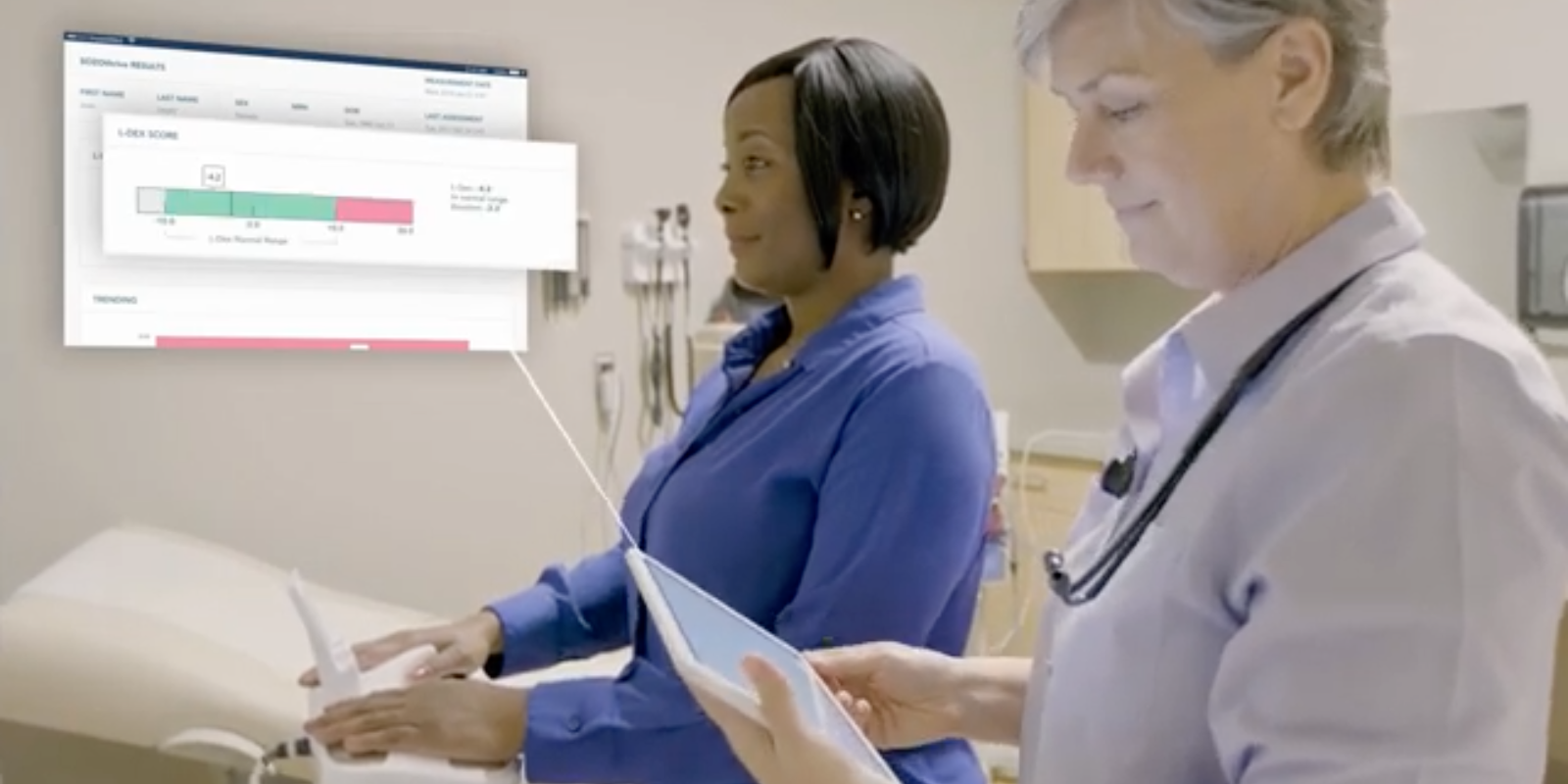
The SOZO Digital Health Platform, a new device in use at the CU Department of Surgery, tests for lymphedema by measuring bioimpedance — the difference in water content between affected and unaffected extremities. Patients step onto the device as they would a scale, place their hands on a pair of sensor pads, and get a reading in seconds.
“Recommendations recently came out to use bioimpedance as the gold standard for measuring lymphedema, which is what we're doing by getting the SOZO machines in our breast cancer clinics,” Egan says. “We can use this as our standard of care to measure and track lymphedema in all of our patients. It's important, because if we catch lymphedema early, then it's much easier to treat. We want to manage it early, before it becomes progressive and irreversible.”
From managing symptoms to reversing the problem
Most patients with lymphedema will work with a lymphedema therapist to reduce swelling through compression, pumping, and manual drainage, but those methods are primarily to treat the symptoms of the condition, Egan says. In recent years, surgeries have been developed that can improve and reverse lymphedema — or even prevent the condition from developing in the first place.
“That's what I do in my practice, is surgeries to prevent lymphedema when lymph nodes are removed by rerouting the lymphatic system,” she says. “At the time of lymph node removal or after lymphedema has developed, I can reroute the lymphatic channels or transfer lymph nodes from another area in the body to rebuild that lymphatic system. It doesn't work in all patients, but in most patients, it at least stabilizes the disease. In some patients it will actually reverse or cure their lymphedema.”
Invasive and not so much
The surgery to move lymph nodes from another part of the body, called a lymph node transfer, is more successful at curing lymphedema, Egan says, but it’s also a more invasive surgery that requires several days of in-hospital recovery.
“I can transfer lymph nodes either from the abdomen, the groin, the back, or the neck,” she says. “I move those into the affected area and reattach the blood vessels with a surgical technique called microsurgery to help the transplanted lymph nodes to survive.”
The surgery to reroute the lymphatic channels, known as a lymphovenous bypass, is a minimally invasive procedure that can be performed once lymphedema has developed — or long before it has the chance to develop.
“Lymphovenous bypass is done through really small incisions, about a centimeter long, using a very high-powered microscope,” Egan says. “Increasingly, I am doing that surgery immediately following the lymph node removal by the cancer surgeon, which prevents lymphedema from ever occurring. That's really the next frontier, because lymphedema is so difficult to treat. Prevention is key for these patients, and we're working to optimize that prevention.”
More accuracy, less time
The addition of the SOZO machine, she says, helps the surgeons track how well their prevention efforts are working.
“It makes a huge difference for us,” she says. “The reliability and consistency of measurements helps us pick up very subtle changes over time that we may have missed with the more rudimentary measurement systems that we were using previously. That's key for being able to catch lymphedema early and get patients into treatment early.
“It's also really simple to use, so that decreases the amount of time that it would take our nurses or physical therapists to do those measurements, and it allows them to have more time for patients.”
Featured image: A patient steps onto the SOZO Digital Health Platform. Photo courtesy of ImpediMed.



.png)
.png)