Each year, since 1987, the President of the United States has issued a proclamation designating the month of March as Women’s History Month. It is significant that the leadership of our country recognizes the importance of reaffirming the historical accomplishments of women with this annual proclamation.
Generations of women have endured hardships, exclusion, and discrimination and despite these challenges have furthered equity and equality in our communities. As a nation, we have made great strides in medicine, technology, social justice, and much more through their unwillingness to surrender their dreams and goals.
We would like to take this time to highlight a few of the great women and their work in the CU Department of Surgery.
Living-Donor Liver Transplant Recipients Gain an Average of 13 to 17 Life-Years Following Surgery
 Research recently published in JAMA Surgery demonstrates that living-donor liver transplant (LDLT) recipients gain an additional 13 to 17 life-years following their surgery compared with patients who remain on the donor waitlist.
Research recently published in JAMA Surgery demonstrates that living-donor liver transplant (LDLT) recipients gain an additional 13 to 17 life-years following their surgery compared with patients who remain on the donor waitlist.
"The really staggering part of the study was that we determined that the survival benefit is not something that increased by several months or even a year or two. The benefit that the patient can expect to gain is 13 years or more,” says Elizabeth Pomfret, MD, PhD, chief of transplant surgery and the senior author of the study.
Improving Treatment for Infants With Cleft Lip and Palate
 Kristen Lowe, DDS, MS, an assistant professor of plastic and reconstructive surgery, has received a grant from Align Technologies, the company that makes the Invisalign tooth-straightening system. The grant will support Lowe in developing more efficient ways to treat infants with cleft lip and palate.
Kristen Lowe, DDS, MS, an assistant professor of plastic and reconstructive surgery, has received a grant from Align Technologies, the company that makes the Invisalign tooth-straightening system. The grant will support Lowe in developing more efficient ways to treat infants with cleft lip and palate.
“In the first few months of life, we can take a wide cleft and minimize the deformity. We bring the gum segments together, the lip segments together, and we shape the noses in these infants in preparation for their first surgical repair, which is traditionally at three to six months of life. The goal is to set up the patient for the best surgical result possible.”
Reducing Catheter-Caused UTIs in Surgery Patients
 When they realized their number of patients with urinary tract infections caused by urinary catheters was tracking above the national average, urologic oncologist Janet Kukreja, MD, and Shannon Bortolotto, APRN, clinical nurse specialist at UCHealth University of Colorado Hospital, knew they had to take action.
When they realized their number of patients with urinary tract infections caused by urinary catheters was tracking above the national average, urologic oncologist Janet Kukreja, MD, and Shannon Bortolotto, APRN, clinical nurse specialist at UCHealth University of Colorado Hospital, knew they had to take action.
The pair pioneered a perioperative quality improvement project to look at how — and when — urinary catheters were placed and removed, even considering whether catheters are needed for some operations. As UTIs can be deadly, especially for older patients, it was an important issue to address.
Surgical Resident Wins Award for Best Cardiac Presentation

Cenea Kemp, MD, a general surgery resident in the Department of Surgery at the University of Colorado School of Medicine, took home the award for Best Oral Cardiac Presentation at the annual meeting of the Eastern Cardiothoracic Surgical Society in October 2022. Kemp was recognized for her research titled An Analysis of Aortic Remodeling in TEVAR for Aortic Dissection: Balloon Flap Fracture vs. the Traditional Method.
Research Finds that Life-Saving Intervention Is Not Risk-Free in Pediatric Patients
 Blood transfusion is a vital and life-saving intervention in a broad range of scenarios, from trauma response to cancer treatment. However, it is not entirely without risk. Research published in 2022, finds that blood transfusion is associated with adverse outcomes – including infection and higher rates of tumor recurrence – in pediatric solid tumor oncology patients following surgical removal of the tumor.
Blood transfusion is a vital and life-saving intervention in a broad range of scenarios, from trauma response to cancer treatment. However, it is not entirely without risk. Research published in 2022, finds that blood transfusion is associated with adverse outcomes – including infection and higher rates of tumor recurrence – in pediatric solid tumor oncology patients following surgical removal of the tumor.
“Blood transfusion is obviously hugely important when used in the appropriate clinical scenario, but there are some downsides,” says study author Shannon Acker, MD, assistant professor of pediatric surgery.
Surgery Team Develops Protocol to Lower Number of Aspiration Events
 Surgical patients under the care of clinicians at the University of Colorado Department of Surgery are at lower risk of complications brought on by an aspiration event, thanks to a new patient safety protocol led by the Office of Quality & Clinical Effectiveness of the Department of Surgery, as reported by Viviane Leite Abud, MD, a quality and executive leadership resident in the department.
Surgical patients under the care of clinicians at the University of Colorado Department of Surgery are at lower risk of complications brought on by an aspiration event, thanks to a new patient safety protocol led by the Office of Quality & Clinical Effectiveness of the Department of Surgery, as reported by Viviane Leite Abud, MD, a quality and executive leadership resident in the department.
CU Surgery Faculty Member Receives DOD Grant to Study Transplant Rejection Biomarkers

Christene A. Huang, PhD, a professor of plastic and reconstructive surgery and transplant surgery in the Department of Surgery, is part of a research team that recently received a grant from the U.S. Department of Defense to study noninvasive biomarkers of VCA rejection that would allow doctors to more quickly identify potential signs of rejection and adjust immunosuppression as necessary.
Medical Student Anna Lee Receives ARCS Scholarship
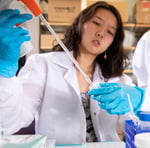 ARCS Foundation, a national nonprofit dedicated to supporting academically outstanding students in science, engineering, math, technology, and medical research, has awarded a $7,500 scholarship to Anna Lee, a second-year medical student.
ARCS Foundation, a national nonprofit dedicated to supporting academically outstanding students in science, engineering, math, technology, and medical research, has awarded a $7,500 scholarship to Anna Lee, a second-year medical student.
Lee was recognized specifically for her work in the lab of Kia Washington, MD, a professor of plastic and reconstructive surgery whose research is devoted to restoring vision through whole eye transplantation.
Study Could Lead to Better Education and Treatment of Sexual Health for Breast Cancer Patients
 A new study led by Sarah Tevis, MD, assistant professor of surgical oncology, found that more than 70 percent of breast cancer patients have reported changes that affect their sexual health during and beyond treatment.
A new study led by Sarah Tevis, MD, assistant professor of surgical oncology, found that more than 70 percent of breast cancer patients have reported changes that affect their sexual health during and beyond treatment.
"More than 3.8 million breast cancer survivors live with permanent or temporary physical and psychological consequences of treatment that impact their sexual health. However, there is limited data that advises providers on the preferred format and timing of sexual health education,” said Tevis.
CU Research Shows That Telehealth Follow-up After Gall Bladder Surgery is Just as Effective as In-Person Clinic Visits
 A research study by Danielle Abbitt, MD, a resident in the Department of Surgery, shows that a protocol that started as a necessity during the COVID-19 pandemic has evolved into a time-saving step for patients recovering from surgery.
A research study by Danielle Abbitt, MD, a resident in the Department of Surgery, shows that a protocol that started as a necessity during the COVID-19 pandemic has evolved into a time-saving step for patients recovering from surgery.
"Based on my clinical experience seeing patients, my hunch was that the results would be similar between telehealth and a clinic visit,” says Abbitt, who also conducted a similar study on patients who undergo surgery to repair an inguinal hernia.
Most People Diagnosed with Cancer Seek Information Even Before Their Appointments
 Research authored by Camille Stewart, MD, assistant professor of surgical oncology, shows that 74% of cancer patients surveyed sought information before a visit, and a large majority of those who searched for information got it from at least one non-validated source.
Research authored by Camille Stewart, MD, assistant professor of surgical oncology, shows that 74% of cancer patients surveyed sought information before a visit, and a large majority of those who searched for information got it from at least one non-validated source.
“As health care providers, we need to be asking ourselves whether we have the trust of our patients, and if we don’t, is it because we’re not providing them the information they’re seeking?” says Stewart. “We want to be the source for information and resources that patients know they can turn to.”
Socially Vulnerable Colectomy Patients Are at Greater Risk for Post-Operative Complications
 Patients who come from socially vulnerable backgrounds are at greater risk for complications following colon surgery, according to a study, led by Heather Carmichael, MD, a general surgery resident in the CU Department of Surgery. Carmichael analyzed data from five UCHealth hospitals relating to patients who had a colectomy, a surgical procedure in which all or part of the colon is removed, between 2012 and 2017.
Patients who come from socially vulnerable backgrounds are at greater risk for complications following colon surgery, according to a study, led by Heather Carmichael, MD, a general surgery resident in the CU Department of Surgery. Carmichael analyzed data from five UCHealth hospitals relating to patients who had a colectomy, a surgical procedure in which all or part of the colon is removed, between 2012 and 2017.



.png)
