It’s only in the last few decades that neuroglia, a diverse group of cells found in the brain that perform a variety of functions to support neurons, have been the subject of research. Prior to that, brain research focused heavily on the role of neurons.
But as investigations continue, scientists increasingly suspect that these cells, often called glia cells or “nerve glue,” may play an important role in psychiatric illnesses, such as depression and schizophrenia.
“When we think of the brain we’re usually thinking about neurons, but that’s only about 50% of what makes up the brain,” says Sukumar Vijayaraghavan, PhD, professor of physiology and biophysics at the University of Colorado School of Medicine, who works at the intersection of neuroscience and society and previously led a lab dedicated to studying the brain’s signaling mechanisms.
The other cells, neuroglia, were believed to function as brain’s janitorial staff, keeping the environment appropriate for optimal neuronal signaling. Then, scientists discovered that neuroglia have their own signaling system different from the electrical signals neurons give off. Glia cells have calcium signals.
“We started wondering what all these cells do,” says Vijayaraghavan, who first took up an interest in glia cells more than 20 years ago.
As it turns out, a lot.
‘Bringing neuroscience into psychiatry’
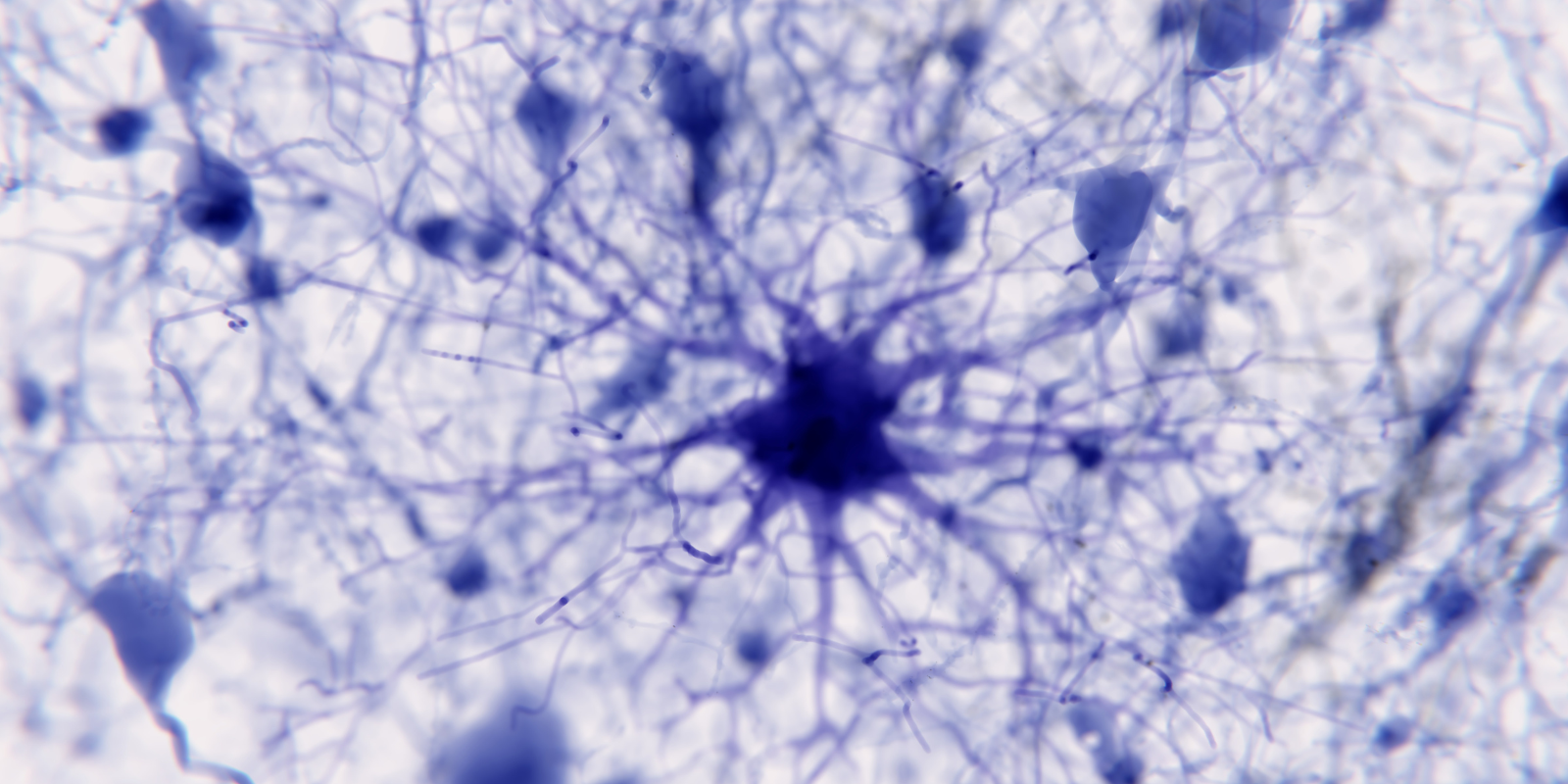
A subset of neuroglia, called astrocytes, seem to be intricately connected to how the synapses work in neurons, and because these cells play a role in brain’s stress response, it’s possible that they are connected to some mental health conditions.
“Calcium signaling was the key impetus to this field in the sense that we found that they have elaborate mechanisms of signaling to each other, to the neurons, and to the blood vessels in the brain,” Vijayaraghavan says. “We previously thought they were non-excitable cells, but it’s actually a unique form of excitability.”
In a 2017 study, researchers in China showed that when astrocyte function is compromised, animal models tended to develop depression-like symptoms. Vijayaraghavan and Andrew Novick, MD, PhD, assistant professor of psychiatry, write in a recent commentary that this is just one example of how glia cells “seem to play a critical role in psychiatric illness.”
“Not only do astrocytes from individuals with psychiatric disorders have different characteristics than those of healthy control participants, but there are also differences based on their clinical profiles,” they write in the essay.
“For example, one study enrolled individuals with schizophrenia who had either responded to or failed a trial with clozapine (an antipsychotic medication). Astrocytes from both groups had deficits in glutamate signaling. The cool part is what happened next: When they exposed astrocytes to clozapine, glutamate signaling normalized—but only in the group of clinical responders,” they continue.
Better understanding of neuroglia could add value in clinics in other ways, too.
Many psychiatric disorders are primarily described in terms of symptoms. The problem with that, researchers say, is that there may be many reasons for those symptoms.
“We're bringing neuroscience into psychiatry in the sense that it's thinking more in mechanistic terms as to what is specifically happening, rather than just relying on symptomatology,” Vijayaraghavan says.
Technology and the future
Novick says it’s important to be able to explain to patients why they’re experiencing psychiatric symptoms and what might be malfunctioning in the brain. So far, that can be difficult to do.
“If you went to the doctor with a stomachache and they only responded with a medicine that could fix the stomachache but not what actually caused the stomachache, that wouldn’t be satisfactory,” Novick says. “That’s not a proper understanding of things, and so we’re trying to figure out what’s causing these psychiatric diseases, not just how to treat them.”
Fortunately, investigating glial cells may help meet both of those aims.
“From all the data we have, we know that there seems to be a connection between astrocytes and depression,” Novick says. “This means there’s likely some impact from drugs used to treat depression, and so that’s an important aspect of how understanding these cells influences psychiatry.”
New technology is allowing deeper investigation into glia cells. Scientists can now take a person’s skin or blood cell — which is easier to obtain than a glial cell — and program it into an embryonic-like state and then turn it into the cell of interest.
“We find a lot of astrocytic markers that are correlated with diseases like depression. That prompts questions of whether that gives us a diagnostic or even a predictive tool to look at what these astrocytes are doing and what causes the depression,” Vijayaraghavan says.
In the future, this work could help develop personalized treatments.
“We could take a cell from a person with schizophrenia or depression, make astrocytes and figure out the dysfunction and design a therapeutic with the individual in mind,” Vijayaraghavan says.