Although interstitial lung disease (ILD) is a common manifestation of rheumatoid arthritis (RA), it is a difficult condition to diagnose. By the time ILD is visible in a CT scan, it is often at an advanced state and difficult to treat.
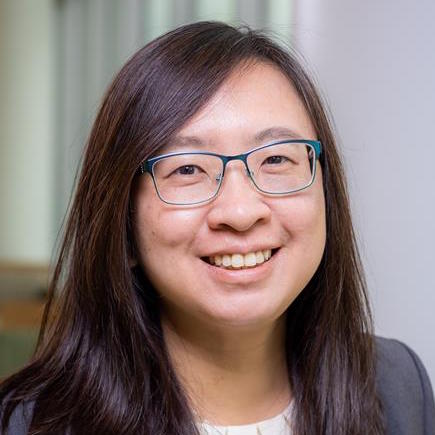
Fan Zhang, PhD, an assistant professor of rheumatology in the University of Colorado School of Medicine, recently received a grant from the PhRMA Foundation for her research aimed at finding an approach to diagnose and treat RA-associated ILD earlier.
Using machine learning — computer systems that use algorithms and statistical models to analyze and draw inferences from patterns in high-dimensional data — she plans to analyze millions of single cell profiles from the joint and lung tissue of patients with RA and ILD to see if there are common connections between the two. The Zhang lab research takes place through the CU School of Medicine as well as the Center for Health AI (Artificial Intelligence) on the CU Anschutz Medical Campus.
“By comparing the cell profiles between those two tissues, we will be able to predict the shared pathogenic features,” Zhang says. “They could be genes, transcriptional factors, or migrating molecules. We hope to reveal novel non-invasive ways to identify progressive RA-ILD through identification of markers in blood, as well as potential transcriptional regulators that drive the inflammatory cell populations. These can be further targeted to stop inflammation in patients with RA.”
The joint-lung connection
ILD is characterized by progressive scarring of lung tissue that affects a person’s ability to breathe and get enough oxygen into their bloodstream. For many, the damage is irreversible, though medications can slow it down. In people with RA, ILD is a leading cause of morbidity and mortality, detected in up to 60% of patients. RA patients with ILD have three times the risk of death compared to those without the disease.
Zhang’s research looks specifically at myeloid cells, a major source of cytokines that play an important role in tissue inflammation in RA. Her previous studies of RA and RA-ILD lung disease revealed a shared myeloid population that may represent a key pathogenic population linking these two inflamed tissues, highlighting the need for a greater understanding of the pathogenic connections between the joint and lung.
“With this grant, we are using the theory of system biology and machine learning to help with translational medicine,” Zhang says. “An improved understanding of the mechanisms that underlie rheumatoid arthritis targeting the joint-lung axis and tissue-blood comparison may help develop therapies to better treat rheumatic diseases in the future.”
Personalized solutions for autoimmune conditions
The Zhang lab has related research funding through the Accelerating Medicines Partnership — a public-private partnership between the National Institutes of Health, the U.S. Food and Drug Administration, and pharmaceuticals companies — targeted at autoimmune and immune-mediated diseases. Since this is a new area of study, Zhang hopes to build a collaborative team of computational biologists and postdocs to join her to work on this single-cell translational medicine project.
“I feel like there is a need to identify a precision medicine for autoimmune disease, because there are no effective personal treatments currently,” she says. “I think we can use big data to looking at patient cells and more effectively identify accurate targets.”
Zhang’s collaborators on the project include Kevin Deane, MD, professor of rheumatology, and pulmonologists Edy Kim, MD, PhD, and Tracy Doyle, MD, from Brigham and Women’s Hospital in Boston.