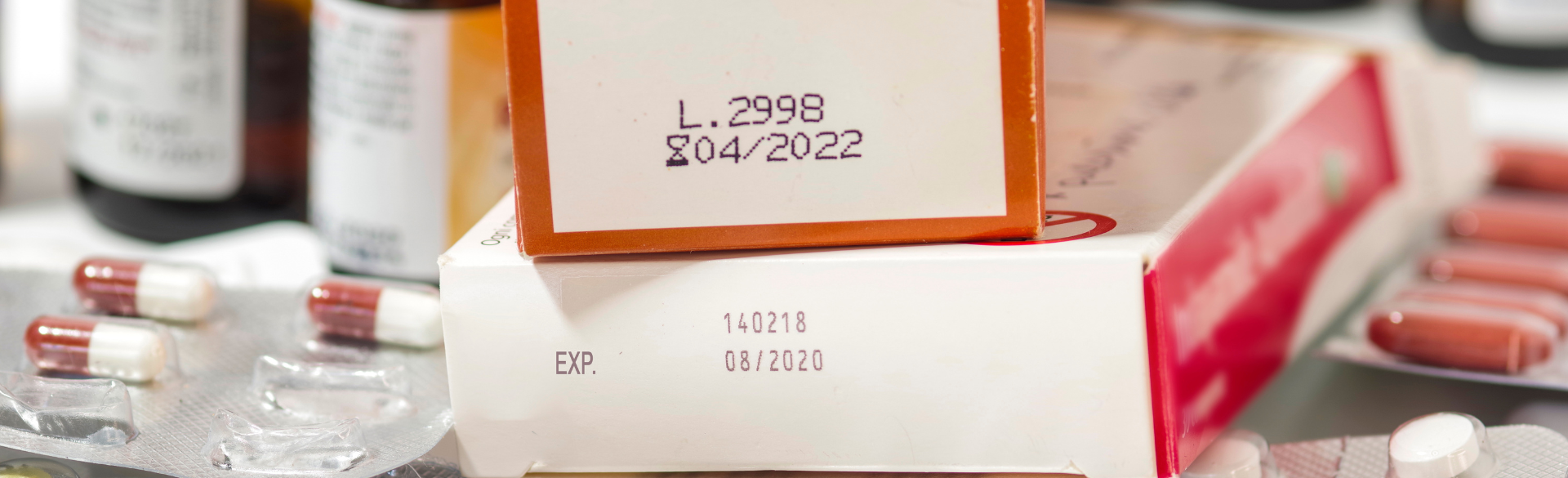
Are drug expiration dates a myth?
They're not a myth, but they're not absolute either. In some cases, they're the best guess from the company as to how long we can safely have these drugs in the hands of patients. In other cases, the drug's stable, but we don't want it hanging around for 20 years, so we pick a reasonable time period, one or five or seven years, to leave it in the bottle or container.
How do drugs break down?
Drugs are chemicals and they're in mixtures – which might be a tablet, a capsule, a liquid formulation or an injectable formulation. With these formulations we can have chemical breakdown, formulation breakdown, or we can have microbial growth. Any of those could limit the dating of a medication.
Most drugs are going to be breaking down based on mostly their exposure to water, hydrolysis by the water. Drug degradation is going to be facilitated by temperature and also by moisture and sunlight. Most of our medicines are coming to us in some sort of an opaque or an amber bottle that will filter out the wavelengths of sunlight that tend to break down drugs. If it gets too cold, water will condense, and you're going to have more water in the product, that would tend to break it down. But at the same time, we don’t want it too hot because chemical reactions go faster when they're heated up.
Formulation breakdown would occur when there are a mixture of chemicals and water, such as in creams and other topical products. You may have a cream or an ointment and that cream or ointment starts out looking very uniform. But when it's left in the wrong conditions then it may separate out, but the medicine is still there and still good.
Then the other thing to worry about is microbial growth. Drugs will be formulated so that they'll be as antimicrobial as possible, but it still depends upon what type of formulation it is. An example of that would be eye drops. The eye is one of the most sensitive areas of the body, so you have this ophthalmic drop that will be isotonic, balanced pH. It's the perfect pH, the perfect salt combination to grow things. In that case, we would keep eye drops in a refrigerator to minimize microbial growth, which is faster as temperatures increase. The drops probably are still good after about a month, but we will typically say, "Don't take any chances after a month, discard that and get new fresh eye drops."
So where is the best place to store drugs to ensure their longevity?
In short: up high, cool and dry.
We think of putting drugs in the medicine cabinet in the bathroom. That's probably not the best place to put them because of the moisture – it tends to heat up a bit when the water's running and the shower's on. Pharmacists will often recommend a linen closet as maybe a better place to keep them. And finally, up high so we are keeping medicines out of the hands of children.
Potentially the worst place you could possibly leave your medicines would be in the glove compartment of your car, particularly in Colorado. Think about the temperature swings we can get here. Even in the winter it can go down to below freezing at night, then up to 70 degrees – and warmer inside your car. These big swings in moisture and temperature are going to cause a drug to break down more quickly.
Should patients be concerned about expired drugs in their home?
So, almost universally drugs are losing their potency, but they're not harmful in and of themselves. Counterexamples are rare, such as tetracycline being potentially unsafe past its expiration date. In my lab, we have studied degradation of drugs, we've done stability studies and I can't think of one of the stability studies we did that actually matched the default dates from the United States Pharmacopeia or the Food and Drug Administration. They're generally set to be very conservative.
One of the things we want to consider when we're advising patients is: What are they using this medication for? Suppose you had a drug like a blood thinner where, if you get too much of it, then you bleed and that's potentially fatal. At the same time if you don't get enough of it, then you clot and that's potentially fatal as well. You want to be very careful with certain classes of drugs and certain types of patients, because they may be right at the margin where these drugs are keeping them alive and just a very slight change in potency could make a profound difference. In these situations, I would not advise patients to use medicines very long beyond their expiration date.
But for most patients, that's not going to be the case. I think it's very safe with an over-the-counter drug to say that's the last date that you can sell those by, it's going to be good for another year. Just to pick a drug almost at random that everyone would have tried, guaifenesin – Robitussin, Mucinex. If that were to be only 95% of what you expect it to be after expiration, as long as what it's broken down to isn't harmful, maybe you're not coughing up as much as you would have with some symptom relief. It's a symptomatic medicine. But the EpiPen, the blood thinners, drugs for patients with seizures or profound heart failure and such, those could be very problematic if they weren't very close to the potency that's expected.
If most drugs are safe after their posted expiration dates, why haven’t the standards changed to extend the expiration dates?
There are a number of issues at play here. Degradation testing can be expensive and usually more conservative dates are chosen to comply with testing requirements, and also to ensure the drug still retains its potency. Because we can’t be sure of storage conditions in a patient’s home, expiration dates err on the conservative side. And last, because of liability concerns, a manufacturer will want to make sure the medication a patient takes is safe and effective.
Stability dating is dependent on drug formulation and packaging, so when anything changes the system goes to established default limitations, which can only be extended through a stability study. We recently published a stability study that allowed one drug to be prepared in ready-to-use packaging rather than dispensed from the manufacturer's packaging. This saved UCH over $150,000 a year and made the drug available to critical care patients in under 5 minutes (previously 26 minutes).
If you're a company, you're balancing marketability, particularly on an over-the-counter medication. The medication will be distributed to the local retailer, such as King Soopers or Walgreens and of course you want sales to go very fast, but you don't want returns. So, you want a drug that's going to have maybe a seven- or 10-year lifespan.
From the patient's point of view, what's the best way to handle this? And the answer is: it sort of depends. If you can afford to throw away your meds and buy new meds, then that's not an issue. If it comes down to not buying food, not buying meds, or taking a med that's a bit outdated, I would say taking the outdated medication is okay. If the expiration date is over a year, I’d suggest they talk with their pharmacist or doctor.

.png)
.jpg)
