What is the current state of 3D printing in dentistry?
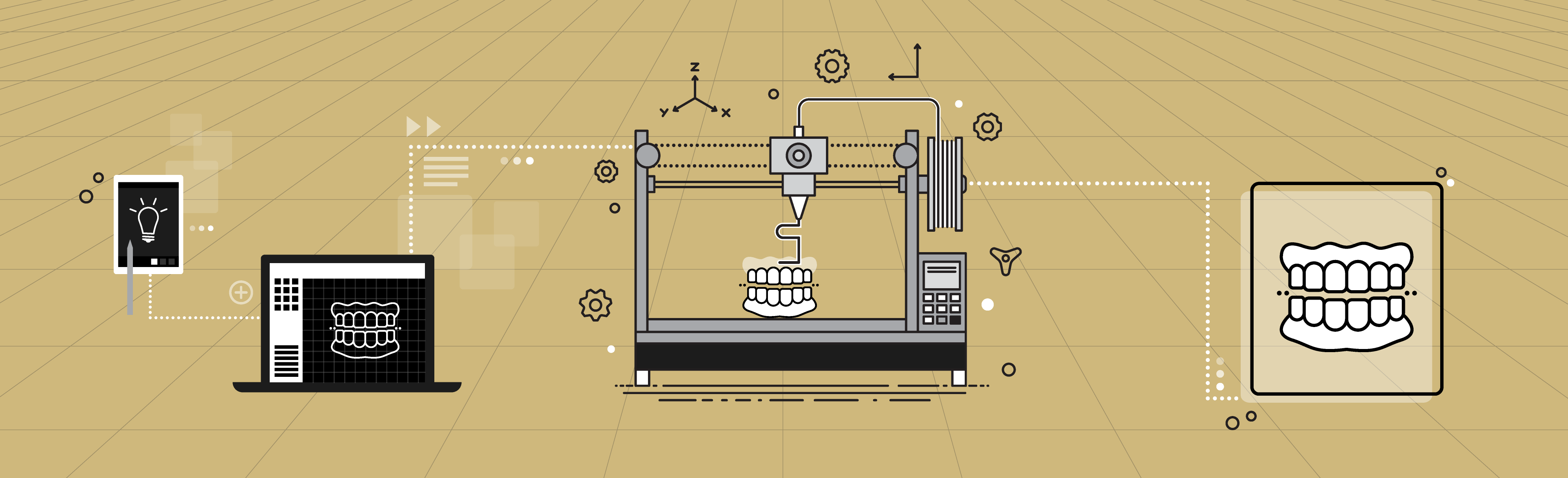
Jeffrey Stansbury, PhD: 3D printing is taking off quite dramatically in the dental profession. While it's still a minority of what’s going on it is rapidly building and is expected to eclipse the reductive milling approach for digitally derived dental device manufacturing in the not-too-distant future.
Right now, the materials are the biggest hold up, and that means that most of what's being printed are dental models – replicas of the patient's teeth for example. So while there’s a big need to achieve higher performance 3D printable polymers that are suitable for long-term clinical function, here we’re trying to leapfrog standard 3D printing techniques and enable the production of fully functional strong and durable dental devices produced via multi-material inkjet printing.
Kyle Sorensen, DDS '25: In dentistry (with current 3D printing), we can do treatment planning, and you can get a record of the oral cavity as well. However, these study casts or molds aren't used for direct dental application – it's just a snapshot of the patient’s mouth.
You can use these casts and molds for various applications, such as designing surgical guides or to create guards that prevent teeth grinding. But the cool thing our project is forwarding is the potential to create intraoral devices, such as: dentures, bridges, or implants - that can be used on a daily basis by patients.
What are the benefits of 3D printing for dental applications?
Stansbury: It has so much benefit in terms of cost for delivery, speed of delivery, efficiency of material use, all sorts of things.
It's the ability to 3D print very high resolution, patient-specific design, which is just ideally suited to what 3D printing does. Mass customization is effectively the terminology for what 3D printing can accomplish. This would be permanent dentures – or removable or partial – as well as crowns and bridges. It’s those materials and the ability to 3D print those materials in very high resolution.
What is 3D inkjet printing?
Stansbury: It’s like an inkjet color paper printer, where you can get any blending of color on the fly. What we're after is to be able to precisely jet droplets of multi-materials to get final unified polymers with localized control of material properties and aesthetic appearance to replicate differences between the gums and the teeth for example.
This is different from conventional 3D printing used now in dentistry – vat-based printing – where you basically create an object layer by layer as it is lifted out of the vat. We are pushing out new materials that well exceed what's possible with current vat-based printing and even more dramatically advancing jettable materials.
Can you explain the science behind these new materials and how they are different from existing 3D-printing materials?
Sorensen: Existing polymeric materials widely used in dentistry typically combine chemically bonded network structure along with secondary interactions that add to strength and toughness. A good example is urethane dimethacrylate (UDMA) where the methacrylate groups react to produce the basic polymer network and the self-association of the urethane groups contributes to the overall performance. However, UDMA doesn’t work for 3D inkjet printing because the association between the urethane groups that is positive in the polymeric state, drives up the ink viscosity in the pre-cure state where the well controlled small droplet jetting must take place.

A simple denture tooth button that was printed as a proof-of-principle demonstration of the new materials being developed at the School of Dental Medicine.
|
Our new CU-patented materials are monourethane dimethacrylates (MUDMAs) that offer much lower viscosities than UDMA before polymerization yet present equivalent mechanical properties in the final polymers. We then coupled our MUDMAs with a second monomer that preferentially interacts with urethane groups to bring the ink viscosity down to the jettable range while also enhancing the reinforcing effects in the final polymers to achieve mechanical properties that appear to be well suited to clinical challenges in dentistry.
The other interesting result is that our new material is more temperature resistant than what’s currently available in the inkjet platform – so it won’t deform in shape when exposed to hot food or liquid. So in addition to being able to stand up more to normal dietary activities, these are very strong and flexible materials that can be accurately constructed using multi-material inkjet printing.
How will determining sizing and fit for these kinds of devices work going forward?
Stansbury: For the necessary digital design of a desired device, there are two approaches that you can take. One is you can do an intraoral scan with an imaging tool. Again, it's not a wand, but you carefully move this around in the patient's mouth and it captures a digital three-dimensional map of the soft and hard tissues there.
There aren't many groups that are doing that right now, but that is another coming attraction for dentistry. What's done now is typically you get a standard dental impression taken and you make a model of the mouth and then you can digitally scan that model.
It adds an extra step. It adds time. At every step along the pathway, there's some degree of uncertainty. So you get less and less precision as you make copies of copies going forward. But that's how you get the three-dimensional digital image that ten allows local or remote construction of the 3D printed device.
Dentists are good at thinking in both the positive and the negative dimension – making a negative model that creates a mold that I can then fill, and it becomes the positive. And this always adds to my level of appreciation for what dentists do – to be able to think in those multidimensional terms, as well as even just being able to work with a mirror and do the right thing in the right place.
Where do you see your research going next on this topic?
Sorensen: I think the next steps would be to test the biocompatibility of these materials and make sure they're safe for clinical application. And then also developing a wider range of materials with not just strong mechanical properties, but ones that are highly flexible, with lower stiffness.
You might want to have materials that are more soft and flexible on the gum surface. The next step would be identifying and developing materials for those applications as well. What's interesting is that with an inkjet 3D printer, you can actually blend different materials with more extreme differences in properties to get an intermediate property.
So you might take something that's really rigid and strong and blend it with something that's a little bit more flexible. This is achievable because the droplets delivered by 3D inkjet printers are picoliter sizes. So you can create materials with graded functional properties that behave more similarly to biologic tissues..
Stansbury: Yeah, what I see coming is the ability to do both the aesthetic and the mechanical blending along with all sorts of different engineering aspects. So we can make something stiff in one direction, but flexible in the other, which again is not something that's doable in any of the other current modes of material manufacture.
This is just opening lots of doors where design engineering, materials science and the 3D print processing can all be brought together and just have some appliances for patients that are cost effective, rapidly developed and offer the best materials and performance available. If we can meet that, then we've solved a lot of problems. It’s very exciting.