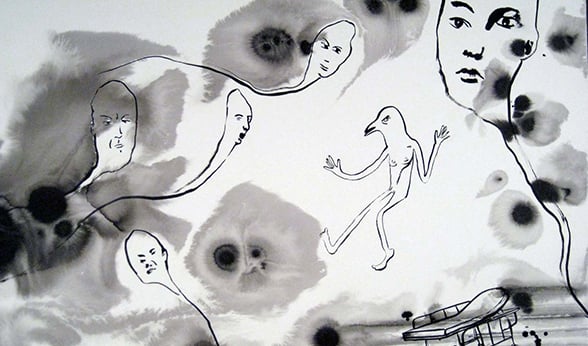
In the picture she drew, the patient drifts above her hospital bed, her body human-like, her head resembling a bird. Shadow-like shapes add an eeriness to a black-and-white backdrop, as ghostly faces float around the room.
The delirium-induced memory of a woman’s days in an Intensive Care Unit (ICU) mirrors those of many critically ill patients’, said Sarah Jolley, MD, of the University of Colorado School of Medicine. These lapses into delirious states are common in any ICU, but especially in today’s COVID-exclusive units, she said.
Artist Nancy Andrews highlights ICU-related delirium after her own experience years ago.
Jolley’s talk on the acute brain dysfunction inflicting the sickest COVID-19 patients and boosting their mortality and long-term cognitive disability risk was part of the June 3 Department of Medicine Grand Rounds. “Neurological and Cognitive Sequelae of SARS-CoV-2 Infection” also included David Beckham, MD, of the Division of Infectious Diseases, and Ken Tyler, MD, of the Department of Neurology.
Delirium strikes COVID-ICU patients at high rate
Citing two studies, one out of France and one from Indiana University, Jolley said researchers found between 65% and 75% of COVID ICU patients in their studied cohorts experienced delirium. The dysfunction affects about half of non-COVID ICU patients, said Jolley, assistant professor in the Division of Pulmonary Sciences and Critical Medicine.
At UCHealth University of Colorado Hospital, COVID-ICU patients are routinely screened for delirium, and providers use preventive practices for the condition, which is missed as much as 75% of the time without regular screening, Jolley said. The hospital has also launched a telehealth follow-up clinic for COVID-ICU patients to assess, among other things, long-term impacts of delirium.
“This is even more common the sicker the patients get, with up to 80% of mechanically-ventilated patients demonstrating ICU delirium,” Jolley said.
Hyperactive delirium causes intense agitation, fearfulness and paranoia, with, for example, some patients becoming convinced doctors are trying to kill them, they report later. Of COVID-19 patients with delirium, hypoactive delirium affects about 87%, resulting in more of a calm, withdrawn and unresponsive behavior. Patients can experience a mix of symptoms from both delirium types.
COVID-19 adds risk factors for brain dysfunction
Risk factors include advanced age and history of cognitive dysfunction or alcohol and drug abuse. Metabolic disorders, sepsis, hypotension, prolonged immobilization and some drugs commonly used in the ICU can also boost risk (benzodiazepines, opioids, anticholinergics).
“There are probably also some COVID-specific risk factors that are combining with these known ICU risk factors to increase risk in COVID-positive patients,” Jolley said, citing social isolation as a chief factor.
Sarah Jolley, MD
Delusional memories and post-traumatic stress disorder (PTSD) can plague discharged patients for months. As part of the ICU Recovery Clinic, a multidisciplinary team follows patients and screens for depression, anxiety and PTSD, among other things.
“We’ve seen 13 ICU survivors to date, and amongst those, we’ve seen 77% with a history of ICU delirium of whom 40% have ongoing cognitive dysfunction,” Jolley said.
Screening, continued studies critical
Prevention is key, with several evidence-based practices made difficult by the social-isolation practices required by the COVID pandemic, she said. Those include liberating patients from ventilators as soon as possible, mobilizing patients early in their ICU stay and engaging family members in care.
Families cannot visit, and patients cannot leave their rooms because of infection risk, she said. “Patients also have increased psychosocial stress related to the pandemic itself.”
With ICU delirium an independent risk factor for worse ICU outcomes, increased six-month mortality, and long-term cognitive disabilities, focused care and more research are critical, Jolley said. “We still need to advocate for aggressive screening of ICU delirium to improve outcomes.”
Drs. Beckman and Tyler presented on other COVID-19 effects on the central nervous system, from encephalitis and strokes to Guillain-Barré syndrome and smell and taste disorders. View the entire Grand Rounds in the video below.