While a recent explosion in AI technology has exposed its possibilities to the public with online systems such as ChatGPT and Dall·E, researchers at the University of Colorado Anschutz Medical Campus have been exploring the rapidly evolving technology for years and are beginning to harness its problem-solving powers to change healthcare.
Already, researchers in ophthalmology are showing success in early detection of a leading cause of preventable blindness in premature infants that could break access barriers and help babies around the world. And both of the region’s top hospitals on campus are reducing sepsis deaths, a major killer of patients, through collaborative, data-driven programs that are predicting the disease sooner and saving lives.
“On this campus, we are determined to be a leader in this field,” Chancellor Don Elliman said in his opening remarks of the 2024 spring “Transforming Healthcare: Changing the Practice of Medicine with AI” held on April 4. The chancellor-hosted lecture series showcases top CU Anschutz scientists and their work for the community.
Read more coverage of the event:
“We are proud to have eminent scientists and researchers already here who will lead us in this effort,” he said, noting that university benefactors make their work possible. “In many ways, they already are.”
Providing the right information at the right time
How can computer science and genetics come together to change a patient’s health outcome? Casey Greene, PhD, founding chair of the Department of Biomedical Informatics (DBMI) at the CU School of Medicine (SOM) and founding director of the Center for Health AI, knows that answer better than most.
Consider a sick and fragile patient being treated with chemotherapy, Greene said, using a case study of a 58-year-old man with rectal cancer as an example.
An AI-generated image of a cancer patient. |
The cornerstone of his chemotherapy can cause nausea and vomiting. His doctor orders a medication to prevent these side effects, not knowing the man has genetic variants that make him an ultrarapid metabolizer of the chosen drug – meaning his body will break down the drug so quickly that it will not have the desired antiemetic effect.
At CU Anschutz, thanks to a collaborative project between the Colorado Center for Personalized Medicine (CCPM) and UCHealth, information about these genetic variants is available in the health record alongside clinical decision support that automatically returns the drug order to the doctor with an alert about the drug-gene interaction along with a recommendation for an alternative drug.
“And that’s really important if someone is receiving chemotherapy,” Greene said. “We could go very far down the path and have a course of treatment that is suboptimal. So our ability to put the right information in front of the physician at exactly the right time to make the right decision leads to better care.”
Under CCPM’s biobank study, UCHealth patients can opt in to getting an additional blood draw that is genotyped for the CCPM’s biobank, with select genetic information returned to their individual records. As of April 2024, more than 54,000 patients have received approximately 350,000 genetic results, which have led to more than 8,000 alerts being received by doctors as part of the nation-leading program, Greene said.
Detecting sepsis and saving lives
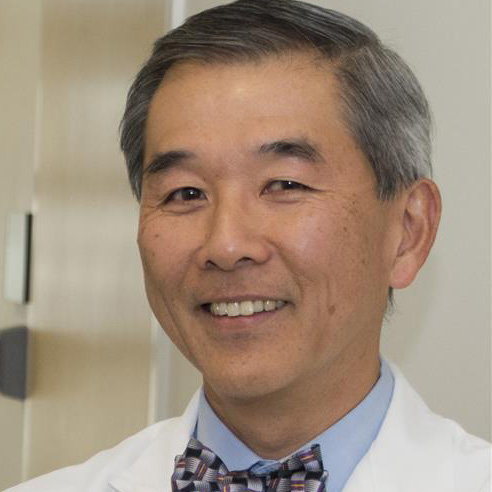
Two AI-assisted programs on campus are targeting sepsis, a deadly infection that persists as a top killer of hospital patients because of its ability to elude clinicians until it’s too late, said CT Lin, MD, professor in the Division of General Internal Medicine and chief medical informatics officer at UCHealth.
“About every hour across the country, 50 people die from sepsis. Hospitalizations for sepsis have doubled in the past 10 years,” Lin said.
He and his team at UCHealth University of Colorado Hospital created a highly sensitive predictive algorithm for adult sepsis, using data from millions of UCHealth patients over the past decade.
While celebrating its accuracy, the team quickly found the method failed at bedside because high sensitivity comes with a downfall: high false-positive rates. Time-strapped caregivers were unable to tolerate the number of false-positive interruptions for the one to two real alerts a day.
The researchers produced a solution, and the UCHealth Virtual Health Center has been making a difference since. Like a command center, the offsite facility is staffed with critical-care experts who monitor multiple screens overseeing all 2,300 beds in the state’s 13-hospital UCHealth system. When those doctors and nurses detect a real alarm, they contact the bedside clinician.

Two guests enjoy food at the Transforming Healthcare lecture series reception in the Anschutz Health Sciences Building before the presentation. |
“This ended up changing the game for us,” Lin said. “Time to antibiotics dropped by 49 minutes. Time to fluids dropped by 77 minutes. There’s been a 35% reduction in code blue/CPR cases and a 20% reduction in transfers to the ICU,” Lin said, adding the program saves over 800 lives every year.
Using AI to update sepsis criteria for kids
Across the street at Children’s Hospital Colorado, doctors also have developed a new tool to head off sepsis in patients worldwide, thanks in part to AI and to international research led by Tell Bennett, MD, MS, attending physician in the pediatric ICU and DBMI vice chair for clinical informatics.
“About 3 million kids die from sepsis every year,” Bennett said, adding that, as with adults, there’s no single blood test clinicians can use to detect it early.
Before his team’s work using machine learning to more easily diagnose sepsis was released early this year, the diagnosis criteria for children were nearly two decades old and non-data-driven. Bennett’s task force spent nearly six years developing and validating new criteria using data from high- and low-resource sites around the world. “It was quite a diverse dataset, and that was really important.”
Their updated criteria are expected to guide many new screening tools ahead and help diagnose sepsis in young patients around the world, said Bennett, adding: “I just spent seven days working in the ICU, and I used it every day.”
Breaking access barriers worldwide
As many people have probably noticed by now, AI algorithms are good at recognizing and sorting photos on cellphones, illustrating imaging capabilities that hold tremendous potential in her field and others, said Jayashree Kalpathy-Cramer, PhD, SOM endowed chair in ophthalmic data sciences and founding chief of the Division of Artificial Medical Intelligence in the Department of Ophthalmology.
For example, her team is part of a current Cancer Moonshot initiative project with the National Cancer Institute that uses AI imaging technology to screen for cervical cancer in hopes of improving diagnosis and overcoming access issues.
With the Moonshot study, women are provided self-sampled HPV tests. If the women are HPV are positive, their cervixes will be assessed by local clinicians and a digital image will be captured. The AI algorithm performance will be evaluated on these images during this phase of the study. In future phases, the algorithm will be incorporated at the point of care.
“Right now, we are in nine countries,” Kalpathy-Cramer said, adding that early data is showing promise.
.png?width=1594&height=1392&name=AI_Graphic(2).png)
AI is an all-encompassing term for artificial intelligence, which includes components such as speech recognition, machine learning (finds patterns from data), deep learning (uses neural networks for recognizing patterns) and generative AI (creates new content). |
Her colleagues are also finding success with an AI-assisted screening program for a leading cause of preventable blindness in premature infants. AI has good ability to diagnose retinopathy of prematurity early, increasing chances of preventing blindness by providing treatment in time. Optimized screening schedules with AI may reduce the stress on babies and can greatly increase access to screening around the world, she said.
New studies are finding AI imaging an effective tool in detecting other eye diseases and much more, Kalpathy-Cramer said. “With a picture of the eye, an algorithm can tell if you are male or female, how old you are, whether you smoke, what your risk of cardiovascular diseases are, and what your risk of Alzheimer’s or Parkinson’s is. The range of possibilities is absolutely enormous.”
Keeping the North Star in mind
A thought-provoking presentation led by Matthew DeCamp, MD, PhD, associate professor in the Center for Bioethics and Humanities and Division of General Internal Medicine, rounded out the event with an important reminder of the many facets and profound challenges of the work ahead.
“What do you think about the idea of an AI crystal ball that can predict your death with shocking accuracy up to four years from now? Is this the job of healthcare?”
As much as that could help doctors, including leaders in the field of palliative care on this campus, DeCamp said: “There are lots of ethics issues around a technology like this one,” he said of a study by social scientists using AI and a huge dataset to predict the likelihood of a person’s death.
As the campus moves forward, CU Anschutz researchers must always keep the North Star in focus, DeCamp said: Is it good for the patient?
And, as AI technology can make mistakes and harbor dangerous biases, healthcare providers must solve those issues and remember the power that new “tools,” from the computer to the automobile, can have on society, DeCamp said. “Unchecked, they change who we are and what we value. It’s up to us to be sure it’s for the better.”
View the event in its entirety (with a surprise AI-themed parody of a Taylor Swift song by one of the experts on ukulele) in the video below:





.png)
.jpg)
