Human anatomy is a universe unto itself – fine-tuned and intricate, and quite delicate. The stakes are very high when a surgeon must navigate, as in the case of a base skull specialist, the labyrinth of miniscule cranial nerves and blood vessels deep within the brain.
There is no room for error in this region – lest the patient’s senses, speech, expressions, cognition or body movements be temporarily, or even permanently, altered. And yet, this specialized field has lacked a comprehensive reference book to guide these extremely nuanced procedures.
“The references in skull base surgery have historically been all over the place,” said Samy Youssef, MD, PhD, MSc, FAANS, editor of the recently published multimedia textbook, “Contemporary Skull Base Surgery: A Comprehensive Guide to Functional Preservation.”
First-of-its-kind reference
Youssef, professor of neurosurgery and Skull Base Surgery director in the Department of Neurosurgery at the University of Colorado School of Medicine, set out to fill the literary gap in his specialty. A renowned global expert and clinician in skull base surgery, Youssef harnessed the expertise of 96 surgeons worldwide, including 15 from the departments of Neurosurgery and Otolaryngology at the CU School of Medicine, to contribute to the textbook.
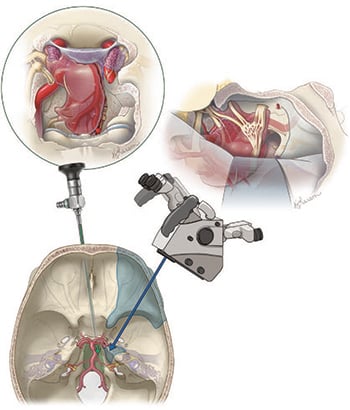
An art illustration of the combined open (right) and endoscopic (left) skull base approach to a complex petroclival meningioma. |
Functional preservation is at the heart of every procedure Youssef performs, and it informs the entire 800-page book. He recalls that when he first trained in skull base surgery, the overwhelming focus was on removing the pathology – the tumor; much less attention was paid to the patient’s post-surgery quality of life.
Fortunately, he said, times have changed.
“Even though these are typically benign tumors, they are intimate to all of these base skull structures that allow someone to interact with the outside environment,” Youssef said. “These are very tiny neuro-vascular structures, which are very sensitive and critical. It takes only a fraction of a millimeter of unnecessary movement, or unplanned movement by the surgeon, to alter somebody’s life.
“And that alters not just the person – it alters their family, their work, their entire life,” he said. “Any damage to that tiny structure, and somebody may not be able to speak or express themselves or interact with their environment.”
Protecting quality of life
So, with the aim to advance patient care – and to protect people’s quality of life – Youssef took the advice of scores of surgeons from across the globe who’ve attended the neurosurgery department’s annual “Microscopic and Endoscopic Approaches to Skull Base Surgery” course. “Young trainees requested this when they came for the course,” Youssef said. “They saw how we do things here at the University of Colorado, and they said we should write a textbook and put this all together.”
The seventh annual conference is scheduled in mid-November, an invitation-only event that draws about 24 surgeons and 12 skull base experts for a three-day, hands-on course at the Center for Surgical Innovation at the CU Anschutz Medical Campus. It’s one of the few facilities in the world equipped for 3D anatomic lectures and allows participants to practice what they have learned in the cadaveric laboratory.
‘Trainees saw how we do things here at the University of Colorado, and they said
we should write a textbook and put this all together.’ – Samy Youssef, editor of
‘Contemporary Skull Base Surgery: A Comprehensive Guide to Functional Preservation’
Within the specialty of removing complex lesions from the skull base has emerged two schools – the traditional open, or transcranial, surgical approach and, more recently, the less-invasive endoscopic (through the nose) method. Youssef sought to bridge this tension by including in each chapter a reasonable discussion that weighs the benefits and shortcomings of each strategy.
‘Depends on the pathology’
“What we endorse here at CU is the combined tools, the comprehensive approach – whether a procedure requires open surgery, or endoscopy, or both,” he said. “It all depends on the pathology and what gets you there in the safest, most efficient way, and ultimately delivers the best outcome for the patient.”
With improvements in radiotherapy, skull base surgeons can now opt to apply radiation to a sensitive structure rather than trying to excise the entire tumor. “It can be detrimental to take the last piece of a tumor out,” he said. “So, functional preservation is a novelty of this book as well. What’s the goal? The goal is functional preservation – whatever it takes to preserve function.”
Each procedure is described step-by-step in the book – which is accompanied by an online version, complete with videos – and enhanced by treatment algorithms. The algorithms are based on tumor morphology, pre-operative clinical status and the goal of maximum functional preservation.
Versatile reference text
Youssef said the book is designed to be a quick, versatile reference that surgeons can use to study tumors and anatomy, but also serves as a surgical atlas that provides the general principles that every skull base surgeon needs to know and explains how to perform each procedure.
Samy Youssef, MD, PhD, is the editor of “Contemporary Skull Base Surgery: A Comprehensive Guide to Functional Preservation.” |
The book describes the importance of developing a multidisciplinary team. Skull base surgeons don’t simply consult with rhinologists, otologists and other specialists pre-surgery; they bring these surgeons into the operating room during the procedure. “That’s a unique part of this specialty,” Youssef said. “We operate as a multi-team, or combined surgeons. These specialists help you to get to the tumors that may be near the smelling nerves, the hearing nerves and other locations in the skull base.”
Another unique aspect of skull base surgery is that, until the compilation of the CU-led textbook, the specialty lacked a compendium of evidence-based best practices applicable to other patient cases. Because the lesions are rare and too complex for patient randomization, there are simply too few cases for controlled studies.
Paying it back
“That’s what makes for another challenge for skull base surgeons,” Youssef said. “You struggled to find an educational tool, or source, to tell you what you need to do in a particular case. Now, with this book, in each chapter a senior neurosurgeon brings personal insight into their successes and failures. A failure can be hard to process, but one that invites future advances in our field.”
Advancing the field is a passion for Youssef, who began the Skull Base Surgery program in 2014. So far, 10 fellows have completed their advanced training, while neurosurgery residents at CU Anschutz gain experience and mentoring while observing Youssef’s surgeries of complex lesions.
“By completing this book enterprise, which carries the name of the University of Colorado, I feel like I’m paying the university back for the opportunity to lead this program,” Youssef said. “I feel it will only build on the university’s already excellent reputation, especially in a rare field like this.”




